SPOTLIGHT IN-DEPTH
Can CO2 monitors help protect healthcare workers from TB?
A recent study published in the journal ‘Clinical Infectious Diseases’ found there was an association between healthcare workers’ exposure to high levels of carbon dioxide and their risk of being exposed to tuberculosis. Elri Voigt unpacks the findings and asks experts how CO2 monitors work, how well they predict the risk of TB exposure, and in which settings they might be most useful.
One of the ways to become infected with tuberculosis (TB) is through airborne transmission – breathing in TB molecules exhaled into the air by a person with infectious TB. A way to decrease the risk of this type of transmission is by improving the ventilation or airflow in an enclosed space and diluting the air and TB molecules in the process. Spotlight has reported on how ventilation can be improved to help reduce the transmission of airborne diseases like Covid-19 and TB.
But how do we know when exactly ventilation in a room falls to dangerously low levels? One solution is to use CO2 monitors.
A recent study set out to test whether there is a correlation between the CO2 levels that a healthcare worker is exposed to and their exposure to TB. The healthcare workers were asked to wear personal CO2 monitors and all worked in settings with a high risk of TB exposure. The study was conducted at Tygerberg Hospital in Cape Town by the Clinical Mycobacteriology and Epidemiology Group, a division of the Molecular Biology and Human Genetics Department at the University of Stellenbosch. Published last year in the journal Clinical Infectious Diseases, it found that there was indeed an association between a high CO2 reading and exposure to TB among healthcare workers in the hospital.
High TB exposure
Grant Theron, a professor of molecular biology and human genetics at the Faculty of Medicine and Health Sciences at Stellenbosch University and primary investigator for the study, says healthcare workers face a huge risk of acquiring TB in the facilities they work in because those facilities are often filled with people who have undiagnosed TB and thus untreated TB, who spread live TB molecules when they exhale, filling the air with TB. Inhaling those molecules can cause TB infection and in some cases eventual TB disease.

Healthcare workers face a huge risk of acquiring TB in the facilities they work in because those facilities are often filled with people who have undiagnosed TB and thus untreated TB. (Photo: Nthusang Lefafa / Spotlight)
The study, according to Theron, looked at 138 healthcare workers in Tygerberg Hospital between August 2017 and June 2019. The sample consisted of mostly nurses and some doctors, with the majority (34%) having fewer than five years’ experience in hospital settings.
He explains that all study participants had an interferon-gamma release assay (IGRA) test when the study started. For this test a blood sample is taken and exposed to dead TB in a petri dish and, based on how the cells in the blood samples react, it can be determined whether the person has been exposed to TB before. The participants were retested a year later. (It is important to note that a positive IGRA test does not mean someone necessarily has TB disease, only that they have been exposed to TB before).
When first enrolled, 74 of the 138 participants had never been exposed to TB before; 37 of the 74 were then chosen to carry personal CO2 monitors with them for a year. A year later, 25 tested IGRA positive.
According to Theron, this means 34% of those individuals who had never been exposed to TB had encountered TB in that timeframe.
“Which means that since joining Tygerberg Hospital, 34% had had their body exposed to live TB, and that’s an extremely high rate,” he says. “Now, that in itself is not a new finding. We know that health workers traditionally carry a huge occupational risk for TB.”
(Photo: today.mims.com / Wikipedia)
Looking for a correlation
This is where the CO2 monitors become important. According to Robin Wood, emeritus professor of medicine at the University of Cape Town, the monitors measure how much CO2 is in the air in a room – this would be related to the size of the room, the number of people in it, how much CO2 they are breathing out, and the ventilation present.
“So essentially, it’s a good marker of per-person ventilation. So it’s telling you how [much] fresh air is being supplied for each individual, but you can also use it to estimate the amount of air that people are breathing from other people… If they’re in close proximity that can give you an idea of how much air exchange there is between people and certainly respiratory diseases are usually dependent on the crowding and the amount of air that you’re breathing from other people, particularly if one of them is infectious,” he explains.
CO2 readings can be used to model the risk of infection with a respiratory disease, but it only indirectly shows the per-person ventilation, according to Wood.
“The main source of carbon dioxide in buildings is air that is exhaled by other people, and the more carbon dioxide in the air, the more exhaled breath. And presumably, if there’s more exhaled breath, there is more TB in the air, assuming you have people with undiagnosed TB in facilities,” Theron says.
Essentially, explains Theron, a low CO2 reading means there is good ventilation in a room, and if TB molecules are present, these are diluted and thus less likely to be inhaled by another person.

A CO2 monitor. (Image: Marco Verch / https://creativecommons.org/licenses/by/2.0/ // Spotlight)
The researchers found that among those healthcare workers who had gone from an IGRA negative to an IGRA positive test, the CO2 readings on their personal monitors were more likely to be higher than those who had remained IGRA negative. According to Theron, the study confirmed the hypothesis that the more re-breathed air or CO2 someone was exposed to, the higher the odds were of them being exposed to TB.
“So that is an association. It’s not a causal relationship, but I think it’s very logical… it suggests that interventions that reduce personal CO2 exposure and improve ventilation can reduce infection in health workers, which is so important for health worker health and protecting what is basically a very rare skill in the country,” he says.
Is it feasible in the real world?
When the study was conducted, says Theron, personal CO2 monitors weren’t readily available off the shelf, but since the Covid-19 pandemic, they have become more available. He adds that they are relatively cheap, at about R1,000 to R2,000 for a consumer-grade monitor.
It is thus feasible to consider equipping healthcare workers with personal CO2 monitors, Theron says.
“The one reason I think it should be a very acceptable and affordable expense is that the cost of having a health worker out of action in a country like South Africa due to TB is so damaging to the system, [and] to that person,” he says.
Implications of the results
The study results have several implications, according to Theron. The first is that ventilation in healthcare facilities needs to be improved. He also suggests mask-wearing for healthcare staff and patients.
“Because we know in South Africa that even if you are coming to the health facility for your HIV treatment, there’s a good chance you have undiagnosed TB. And a good precaution, a good way of preventing TB from spreading, in addition to ventilation, is just wearing a mask. And what’s nice about ventilation and what’s nice about mask-wearing is that those are not specific to TB, those prevent any kind of respiratory infection whether it’s Covid-19 or cold or influenza, or anything,” he says.

Interventions such as CO2 monitors and improved ventilation can help reduce personal CO2 exposure and transmission of airborne diseases such as TB.
The second implication is that the study has shown that a personal CO2 monitor is a tool that can be used to empower healthcare workers and give them the ability to point out areas that are dangerous for them. Giving healthcare workers personal CO2 monitors would act in the same way as a radiation dosimeter used to measure a healthcare worker’s exposure to radiation.
“The thinking was that that really allows health workers to be champions and advocates for their own safety and their own working conditions. Because it’s possible to go and measure CO2 once a year in a stationary place. But if you have something that clips on your belt, which allows you to self-identify as to where risky areas might be, where there is poor ventilation, not only does that allow you to help avoid those areas, but it also allows you to advocate for change within your local environment,” Theron says.
“By improving their working environments, they are also reducing transmission to other patients. And it just really shows that you do not need sophisticated technologies to make these modifications,” he adds.
However, this does not mean that CO2 monitors should be seen as a silver bullet solution to be used in all settings.

Professor Robin Wood. (Photo: Joyrene Kramer / Spotlight)
Not for all settings
Spotlight asked Wood whether CO2 monitors should be installed in public spaces like healthcare facilities or schools. He responded that while this is a useful technology that helps raise awareness of poorly ventilated spaces, it won’t be useful in all settings.
“CO2 [monitors] could tell you that you got a problem [with ventilation], it could be a little battery machine you carry around with you. So, I would be in favour of it being a technology that people would go and use, and you go to a crowded waiting room and check how bad it is. Go to a prison cell, check how bad it is,” he says.
Dr Graeme Hoddinott, a socio-behavioural scientist on TB/HIV from the Desmond Tutu Centre for TB, spoke to Spotlight about the feasibility of using CO2 monitors in schools. Recently, Spotlight highlighted the issue of TB transmission in our classrooms.
He says that theoretically, CO2 monitors could be put into classrooms and could be useful in some circumstances. But cautioned that for many schools in the country, particularly rural ones, there are bigger challenges, like working toilets, optimally functioning school feeding schemes, and educator support.
He adds that in the absence of a CO2 monitor in this kind of setting, we would still advocate that schools keep doors and windows open.
“I mean, use technology, yes. I could imagine in certain circumstances a thing like a CO2 monitor that’s [essentially] like a smoke alarm that goes off and indicates, ‘No, seriously, now you either have to leave the room or open the window’. I see how that could have some programmatic use,” he says. “Implementation in all the thousands of schools in the country would be challenging. Not because we shouldn’t use this tool, but just being cognisant of other things that we know about how the system in the schools is functioning.”
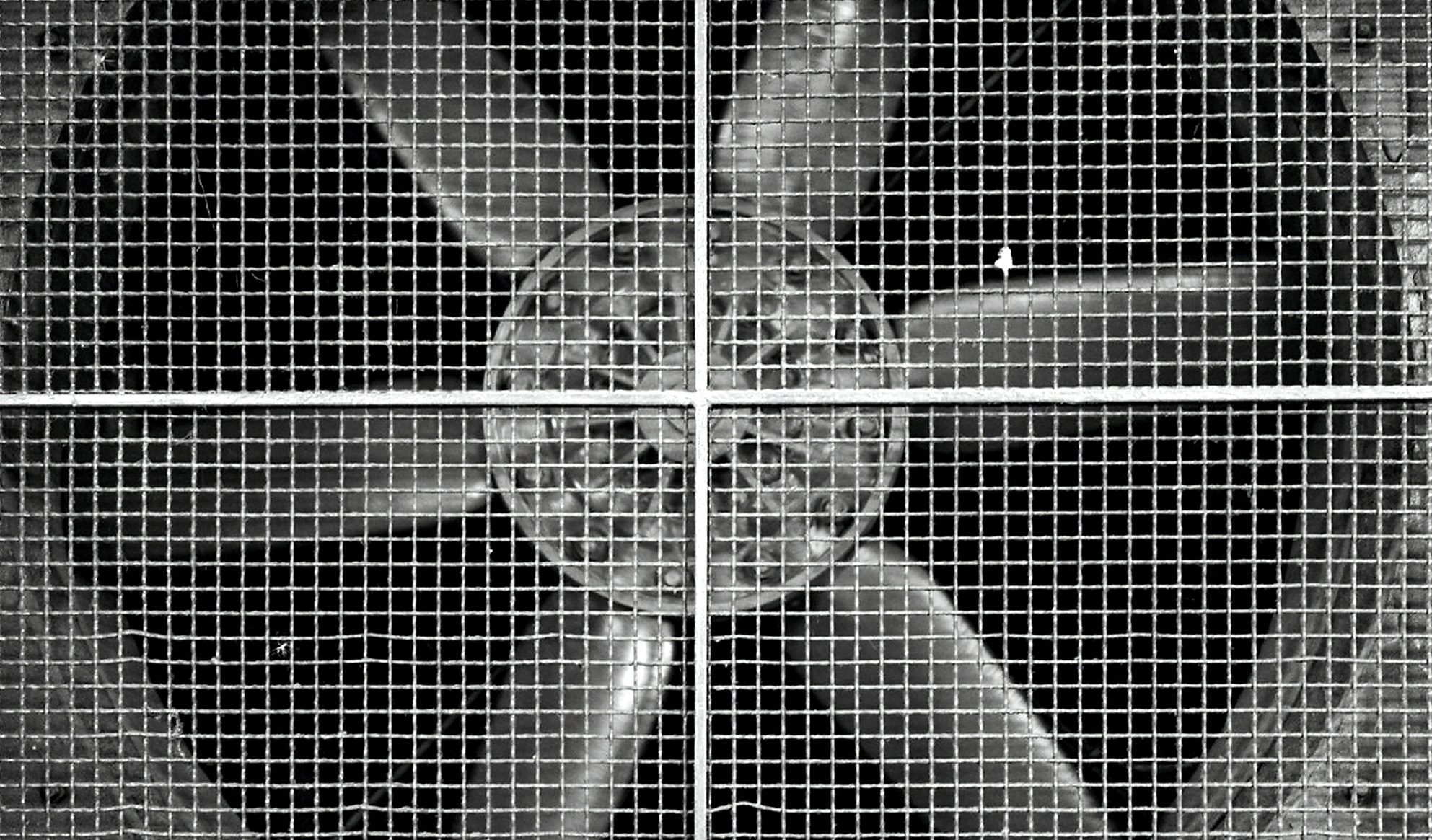
Ventilation plays an important role in preventing the transmission of airborne diseases. (Photo: x1klima / Flickr / Spotlight)
Other tools
According to Hoddinott, there are broadly three ways to reduce TB transmission. First, making TB diagnosis and treatment as easy as possible for people with TB to access reduces the number of bugs breathed out. (People who are ill with TB are thought to become non-infectious around two weeks after starting treatment.) This is followed by reducing the concentration of TB bugs in places where we share air, for example, by wearing masks, opening windows, or having ventilation systems in place. And lastly, prophylactic use of medication, called TB preventive therapy, for those who have been exposed to TB. As Spotlight outlined earlier this year, the eligibility criteria for TB preventive therapy have been broadened dramatically in South Africa.
Wood explains that there are ways to improve ventilation in buildings, but there are some costs involved.
“The solutions [to poor ventilation] have a cost associated with them. If it means the building has to be modified or filtration has to be included in there or ultraviolet light. So those all are costly solutions to a problem that you can define and identify with CO2 monitoring,” he says.
Some of these tools include ultraviolet lights, which can kill TB and other airborne infections; internal air filtration pump that pumps air through filter, or simply introducing more fresh air by opening windows and doors.
“Ultraviolet lights are not that expensive, but they do need to be maintained… then you have to have the ultraviolet light shielded from individuals because normal ultraviolet light is dangerous. [Air] Filtration [systems] have an upfront high cost. They need to have their filters changed at regular intervals [and] they use power and with power outages, they’re not going to work all the time,” Wood says. “There’s no doubt that fresh air ventilation is the best way of doing it, but it requires you to actually design the space right from the beginning with that in mind.” DM
This article was published by Spotlight – health journalism in the public interest.






















 Become an Insider
Become an Insider
A fascinating article and accompanying study.
But, and this is a huge “but”, given the ANC’s demonstrated inability to run anything professionally, it is pie in the sky.