SPOTLIGHT ANALYSIS
Incentives seem to work in private healthcare, so why not in public?

Doing ‘the right thing’ for one’s health, be it eating well, exercising or going for an annual HIV test or blood pressure check, is easier said than done. One way to nudge people to make these ‘right’ decisions is to offer rewards or incentives. Spotlight asks whether aspects of some popular private sector incentive schemes might be worth copying in South Africa’s public sector.
While incentive programmes have made a splash in private healthcare, they’ve hardly caused a ripple in South Africa’s public sector. In fact, the only public sector incentive of any notable scale of which we are aware was the vouchers that were offered to people who got vaccinated against SARS-CoV-2.
Discovery Health Medical Scheme’s Vitality programme is probably the best local example of such an incentive programme.
There have been several scientific studies of cash transfers and other incentives, but the data is relatively limited and the differences between studies were substantial, as indicated in this review of cash transfers for HIV prevention, among others. Evidence from other countries has shown that a targeted public sector incentive programme could yield significant positive results.
The Indian government launched a programme called Janani Suraksha Yojana in 2005, “with the goal of reducing the numbers of maternal and neonatal deaths” using a conditional cash transfer scheme to encourage giving birth in a health facility. In those who benefited from the scheme, there was a reduction of 4.1 perinatal deaths per 1,000 pregnancies and a reduction of 2.4 neonatal deaths per 1,000 live births.
As Spotlight has recently reported, South Africa is doing relatively poorly against its diabetes and hypertension targets and substantially better against its HIV targets. Yet, we can find no evidence that the Department of Health has given serious thought to incentive programmes in these various areas.
Some might argue that the impact of such programmes is unproven and that they are too expensive. No doubt, a carbon copy public sector version of Vitality is wishful thinking. But are there any elements of it worth copying or adapting for the public sector?
“It has always amazed me that incentives are always so okay for rich people like me, on Discovery, but somehow unacceptable for poor people ‘who should do it for their own good’ in the public system,” says Prof Francois Venter, who heads up Ezintsha at Wits University. He describes it as patronising.

Professor Francois Venter from Ezintsha at Wits. (Photo: Supplied)
Venter says that while hugely complex issues like controlling non-communicable diseases (NCDs) and obesity can’t be solved with incentives, they could certainly be added to the very limited toolbox of the existing arsenal being used to prevent disease or death through early detection, testing and screening.
He says incentives “definitely should not be dismissed right off the bat when it comes to the 84% of people who rely on the public system”.
The power of ‘points’
An estimated 60% of diseases across the board are caused by unhealthy lifestyles, according to a 2022 study published in the International Journal of Environmental Research and Public Health. In line with such evidence, Discovery’s Vitality programme is primarily focused on encouraging its members to make healthier lifestyle choices.
“Vitality aims to leverage behaviour change techniques, most notably using incentives, to motivate or nudge members to adopt healthy behaviours,” says Dr Mosima Mabunda, who is the Head of Wellness at Vitality. She says that four core factors are implicated in most NCDs: an unhealthy diet, a lack of physical activity, smoking and alcohol misuse.
The Vitality programme is complex and uses a wide range of incentives and rewards to motivate members, including giving members monetary rebates for healthy food purchases, subsidised gym membership and a comprehensive points-based system that rewards a range of healthy lifestyle choices.
The financial implications of treating common NCDs in South Africa are staggering. (Photo: Supplied)
These points can be converted to cash or used at a range of local retailers. There is an incredible variety of Vitality rewards that range from discounts on flights to discounts at movie theatres.
According to a Discovery report, the “overall impact of Vitality on mortality rates is significant”. By “making people healthier”, they say they have achieved an average reduction in mortality of 13%.
Several experts interviewed by Spotlight point out that most of this data has not been published in reputable, peer-reviewed journals. Even so, it is certainly plausible that Vitality’s annual incentivised health check helps with earlier diagnosis of hypertension, diabetes and even HIV.
Similarly plausible is the idea that points may successfully incentivise some people to exercise more.
Scepticism of the health benefits of other elements of the Vitality programme may well be warranted – it is hard to know without independent analysis.
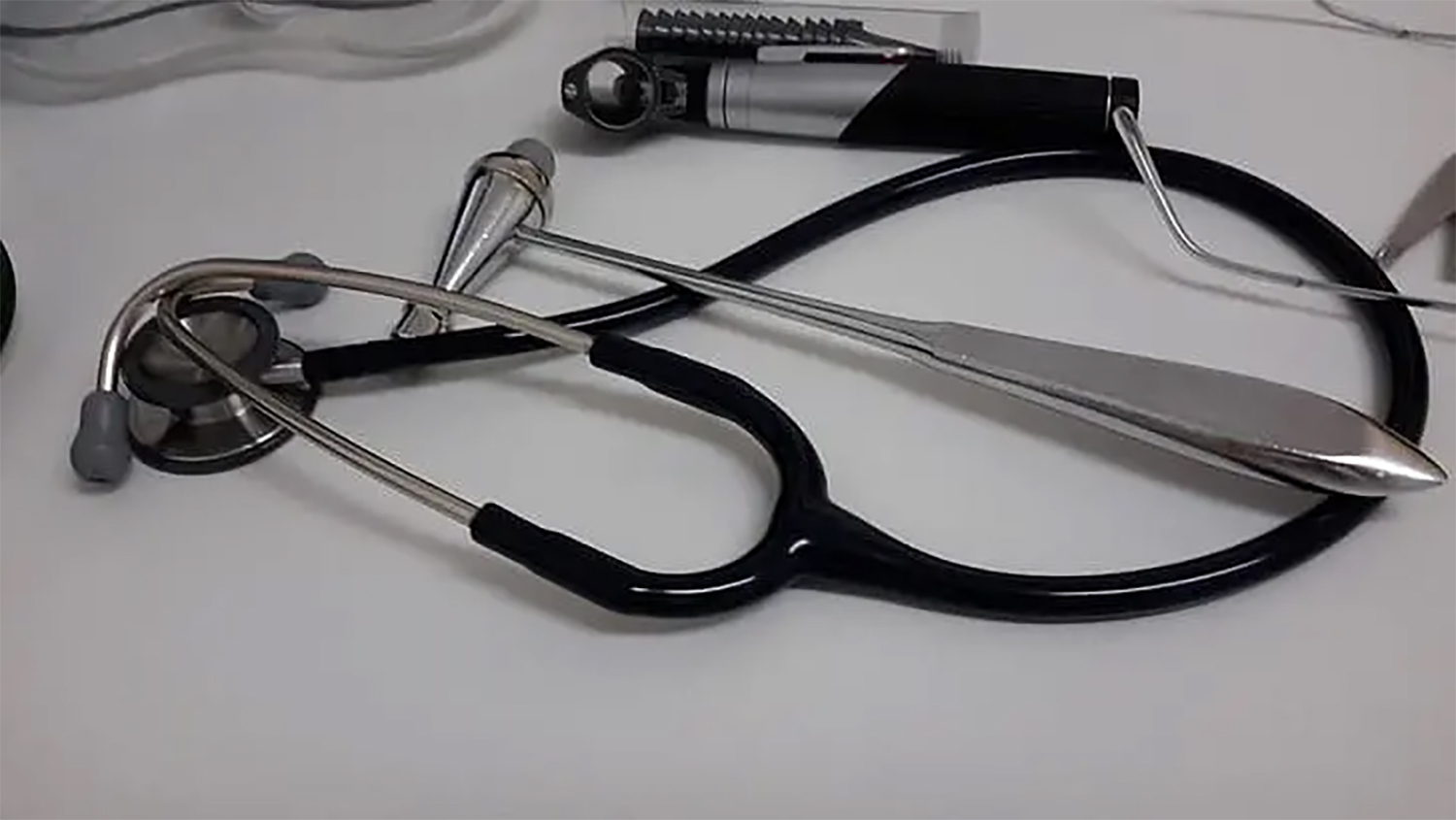
Importance of early detection
The underlying logic of such incentive systems is typically that the savings due to behaviour change or early detection outweighs the cost of the incentives.
Put another way, the private sector isn’t just doing this to help people stay healthy – they are also doing it to save money. The costs and benefits for state-run incentive programmes will obviously look very different, but there may well be cases where the benefits of incentives outweigh their costs.
It is also possible that, in some instances, incentives are needed more urgently by users of the public sector than the private.
As Prof Harsha Thirumurthy, who is an expert on behavioural economics and health incentives based at the University of Pennsylvania, points out, “the majority of Vitality members don’t face barriers like transport costs” or even being located many kilometres away from the nearest state facility.

South Africa is doing relatively poorly against its diabetes targets. (Photo: Bradley Johnson / Flickr)
Late diagnosis or poor disease control has high human and economic costs in both the public sector and private. According to a 2013 study published in the Global Health Action journal, uncontrolled diabetes caused 8,000 new cases of blindness and 2,000 new amputations in South Africa in 2009 alone.
More recent statistics reveal the situation is getting worse.
In 2018, then KwaZulu-Natal MEC for Health, Dr Sibongiseni Dhlomo, revealed that six amputations occur every day – which equates to over 2,100 a year – in that province.
The financial implications are staggering.
For example, a 2022 literature review that looked at the costs of treating common NCDs in South Africa, estimated the cost of treating one person for one year with medication for type 2 diabetes to be roughly between R1,000 and R3,500 in the public sector.
In comparison, the study also looked at the costs of treating common complications of uncontrolled diabetes. For example, diabetes-related renal disease was estimated to cost roughly R67,000 per person per year.
Screening for diabetic retinopathy, an eye condition that causes vision loss, costs between R110 and R370 per person. In comparison, the cost of treating ophthalmic disease in people with diabetes is estimated to be R59,000 per person per year.
These are only the health system costs and don’t include the costs of serious complications and lifelong disability to individuals, families and communities.
Barriers to healthy lifestyle choices
Most experts we spoke to agree that the Vitality programme in its entirety is too complex and expensive to be replicated at scale in the public sector.
Additionally, helping the majority of the population make healthy lifestyle choices, particularly those around healthy diets and physical activity, is a mammoth task and exceeds the ambit and powers of the National Department of Health.
“It’s really important to appreciate that there are so many environmental, social, [and] structural factors that make it difficult for people to quote-unquote ‘do the right thing’ when it comes to health-related behaviours,” says Thirumurthy.
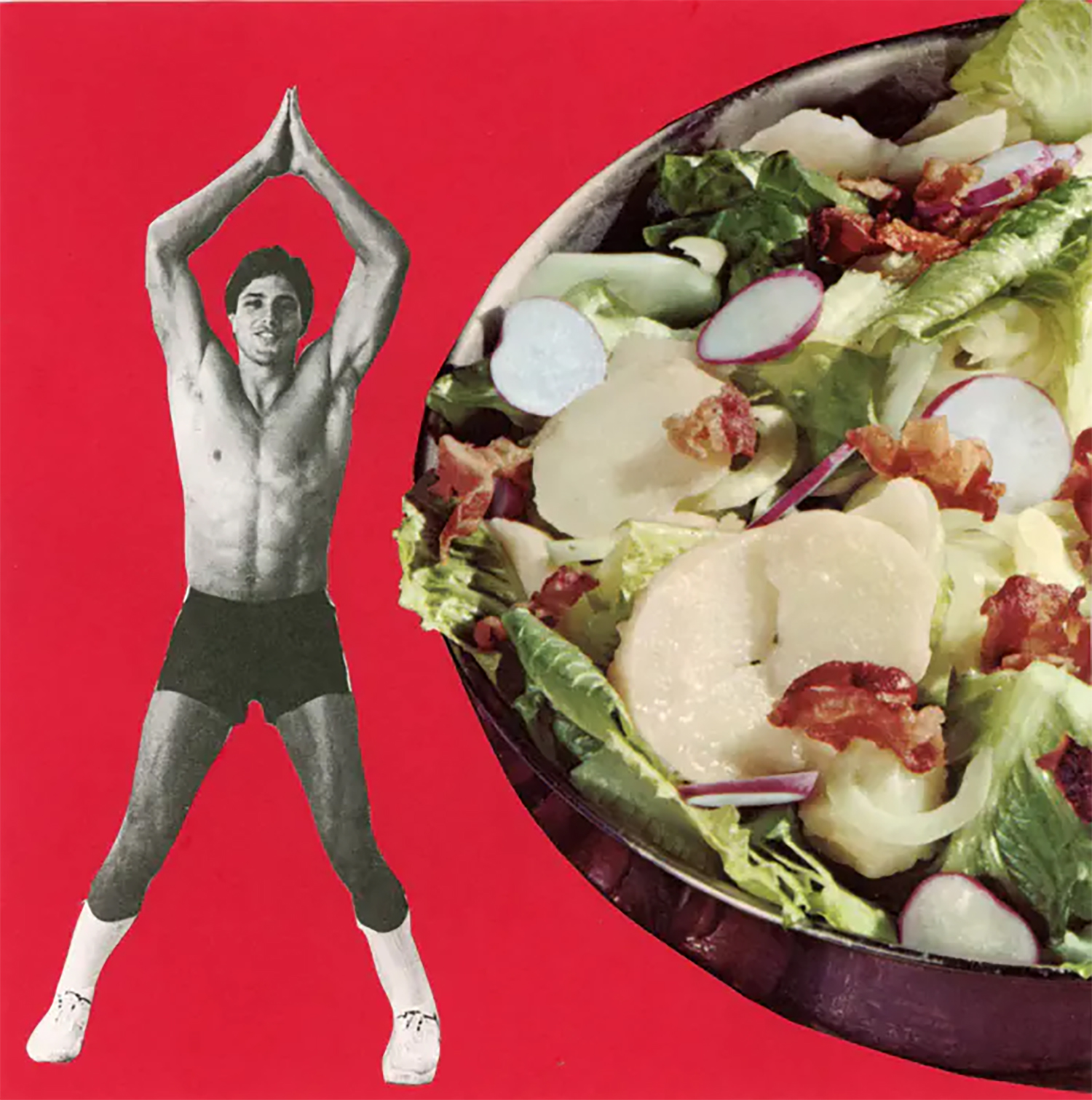
People are often subjected to the advertising of unhealthy food products and many live in environments that make it hard to eat a healthy diet even if they wanted to, one expert notes. (Photo: Tyler Hewitt)
“For example, people are constantly subjected to advertising of unhealthy food products. Many are living in environments that make it hard to eat a healthy diet even if they wanted to.
“To really make a difference, we have to take a step back and identify the overall system-level or structural changes that could be made to influence people’s diets and other health behaviours.
“We need to think about what types of government regulation and policy levers can be utilised to achieve better health outcomes,” says Thirumurthy, who is also the co-founder of South Africa’s first “nudge unit”, based at Wits University, called Indlela: Behavioural Insights for Better Health, which is focused on identifying low-cost behavioural solutions to public health challenges.
As Spotlight previously reported, many of these issues are flagged in South Africa’s recently published Strategy for the Prevention and Management of Obesity in South Africa 2023 – 2028.
But while most experts we interviewed felt the strategy flagged the right issues, there was also agreement that the strategy didn’t set out a realistic plan for dealing with those issues. And not finding ways to deal with these issues is costing a lot of money.

One expert says we need to think about what types of government regulation and policy levers can be utilised to achieve better health outcomes. (Photo: PHM-SA)
In 2018, the public sector cost of treating patients diagnosed with diabetes alone totalled R2.7-billion, “and would be R21.8-billion if both diagnosed and undiagnosed patients are considered”, according to a 2020 report about the health promotion of NCDs published by the South African Medical Research Council.
Moreover, in real terms, it is estimated that by 2030 the cost of all type 2 diabetes cases will soar to R35.1-billion.
According to Thirumurthy, incentive-based interventions represent one creative solution with the potential to help improve health outcomes and reduce the financial burden on the health system in the long term.
“I’m not saying incentives or rewards-based programmes are going to save the day, so to speak. However, they do represent a small but important part of an overall policy package that is necessary to address NCDs. Global experience suggests this policy package should prioritise regulatory interventions, including taxes on sugary sweetened beverages and other unhealthy foods, but incentive-based interventions can certainly be a useful addition to a broader strategy or policy package,” he says.
A public sector annual health check?
Early detection is one area where the public sector could potentially benefit from copying a private sector incentive scheme.
Vitality’s annual health check is a free screening and testing consultation that includes HIV testing, mental health screening, body mass index evaluation, blood pressure check and a blood glucose test, among other things. Members are rewarded handsomely with points, simply for showing up. Critically, these checks are offered at many pharmacies and are thus relatively easy to access.

Early detection is one area where the public sector could potentially benefit from copying a private sector incentive scheme. (Photo: The Open University)
According to Belinda Kahler, Wellness Specialist for Vitality, there is data that suggests the inclusion of a screening questionnaire for depression in their annual health check yields significant benefits for both the scheme and its members. She says that members who complete the screening and are flagged as high-risk are over three times more likely to seek professional help, which “fosters early detection and management which reduces complications and ultimately reduces healthcare costs”.
One way a public sector version of this could work would be for the state to contract with nurses at private sector pharmacies and GPs to provide the checkups in addition to public sector clinics.
This would make it much easier for people to access these checkups and may well boost early diagnosis of diabetes, hypertension and other diseases, especially if an incentive is included.
For this to work, the public sector data systems to facilitate the capturing of measurements and test results will have to be in place, but, presumably, work along these lines is already underway for the NHI data system that is being developed.
Many public sector clients already collect their medicines from private sector pharmacies and some were vaccinated against SARS-CoV-2 at private sector pharmacies – so it won’t be breaking entirely new ground to add checkups to the mix.

Many public-sector clients already collect their medicines from private-sector pharmacies. (Photo: Supplied)
According to Thirumurthy, programmes that are ongoing, requiring daily or weekly action, are not feasible or sustainable for the public health system at this stage as they are too resource-intensive, requiring constant monitoring and reward allocation.
“But incentivising a once-off or annual behaviour, such as going for a vaccination or health check, is not only more likely to succeed compared to daily behaviours like going to the gym or taking a certain number of steps, it is also much more cost-effective and much easier for a government to implement,” he says.
He says addressing healthy lifestyles is incredibly difficult and preventive care interventions represent a more attainable goal for the National Department of Health.
Screening, preventive care and early detection save money and lives, but it is notoriously difficult to get patients to engage in the health system before they get really sick or experience noticeable symptoms. More often than not, patients seek care too late to prevent costly complications.
“Depending on the particular behaviour, test or screening combination that is incentivised, a programme like this could really move the needle on the intended health outcome and equate to money well spent in future averted healthcare costs,” says Thirumurthy.

Experts warn that we will have a collision of comorbidities in the next seven to eight years fuelled by an ageing HIV population. (Photo: Unicef Ethiopia)
Dr Brendan Maughan-Brown, the Chief Research Officer at the Southern Africa Labour and Development Research Unit, points out that “we really are going to have a collision of comorbidities in the next seven to eight years” fuelled by an ageing HIV population.
“All these NCDs are going to become even more burdensome to the health system – already in some areas, over 25% of people over 50 are living with HIV. This is going to be a major challenge for the health system, insurers and the NHI, so thinking about solutions now, including a proposed annual health check or screening, is a good place to start.”
What should incentives look like?
Once-off or annual programmes do not need to be expensive, according to Dr Sophie Pascoe, who is the Indlela co-director.
“They would require a level of coordination, but there are many companies who I’m sure would be willing to come on board as sponsors. The big supermarket chains could subsidise grocery vouchers or incentives could be in the form of airtime backed by one of the big mobile networks, for example,” she says.
These partnerships would “benefit everybody” by encouraging those targeted behaviours, while sponsors would profit from the exposure and an increase in their customer base.
“I think part of the problem is, when we mention the word ‘incentives’, everyone imagines a lot of money and big rewards. But the rewards don’t need to be big or costly,” she says.
Maughan-Brown, who is also an expert in behavioural economics and the behavioural determinants of HIV risk, says that for an incentivised preventive programme to be successful, there needs to be a comprehensive understanding of the various “hassle factors” faced by those who rely on the public health sector.
What would be valuable to people? Transport, airtime, grocery vouchers, child care, paid leave from work or something else?
He says a lot of work would need to be done to understand what rewards will work and there needs to be a level of flexibility because different people will need or value different incentives.
Pascoe, in turn, suggests that a lottery incentive could be added and would be inexpensive to augment an immediate but smaller reward that would be received directly after the health check or screening intervention, for example.
She adds that another difficulty when it comes to advocating for this kind of programme is that tangible benefits or outcomes will only be seen in the long term, while government is more receptive to programmes or policies with clear and quick results.
Venter has similar concerns. He says there is a perception that these programmes are expensive to implement and run.
“But that is only part of the issue,” he says.
“I find it bizarre that I get incentivised left, right and centre by Discovery, yet every time we raise it for poor people, I get told ‘they should be doing it, anyway’. It makes no sense.”

Late diagnosis or poor disease control has high human and economic costs in both the public sector and private. (Photo: Jernei Furman)
As it stands, Venter says that problematic and pervasive perceptions need to be addressed before any incentive-based programme will even likely be considered by policy-makers and government officials, and even international funders, civil society and the media, for that matter.
‘Already incentivised’
National Department of Health spokesperson, Foster Mohale, told Spotlight that his department “is not against incentivisation, but each preventive programme has its own issues and each community of health system user has different incentives for staying well”.
He agrees that the “public health benefits of health checks and health screening” have the potential to “result in early detection and reduced costs to the health system”.
However, Mohale says that these services are already incentivised and that considering interventions inspired by Vitality is “inappropriate”.
Asked about the nature of the current public sector incentives, he said, “[It] depends on what one sees as an incentive! For me, a gym membership, Fitbit, express check-in queue or cheap flights are of no value and I regard them as an insult. For others, they rush to ‘benefit’. For the majority of South Africans, a visit from the [community health worker] is the incentive.”
Mohale argues that, by definition, incentive “means inducement, motivation, motive, reason, encouragement” and that, “in the true spirit of incentives”, “testing and screening services are incentivised through health promotion in ALL public health clinics, and in school health programmes”.
He says that “the massive programme for HIV testing [is] incentivised through free testing [and] specific clinics”.
Mohale adds that the department offers another incentivised programme in the form of adherence clubs, where groups of about 30 people who are on chronic medication meet regularly, share their experiences and receive some screening and counselling from healthcare workers. DM
Prof Francois Venter is quoted in this article. Venter is a member of Spotlight’s Editorial Advisory Panel. The panel provides the Spotlight editors with advice and feedback on the quality and relevance of Spotlight’s public interest health journalism. The Spotlight editors, however, remain editorially independent and solely responsible for all editorial decisions. Read more on the role and purpose of the panel here.
This article was published by Spotlight – health journalism in the public interest.





















 Become an Insider
Become an Insider
And who, pray tell, will pay for these incentives? Public healthcare funds are already plundered by the anc, setting money aside for incentives will only incentivize the criminal cadre deployees to steal it
As top tier Vitality members, we receive many R’000s in cash back and gym savings etc., etc., which largely covers our premium, and, as pensioners, is a significant bulwark against inflation.
Mohale sees this as ‘of no value and … regard(s) them as an insult’.
Yeah, right.
Members of wellness programmes pay significant membership fees every month and membership is voluntary. Not sure whether that would work for public health care.