President Cyril Ramaphosa was widely praised after he announced a national lockdown for 21 days from 27 March until 16 April. When the lockdown was extended by a further 14 days the response was notably less complimentary. The five-week hiatus will have devastating consequences for the economy — particularly for small businesses which do not have the capital to see them through the break in activity.
Small businesses are important job-creators in an economy with unemployment (narrowly defined) approaching 30% and, including discouraged workers, in the region of 40%.
The impact of this lockdown on the South African economy (and the global economy) will be significant and lasting. It’s a long road back, and there’s no clarity on what the future holds.
And the question remains: is this enough? Should the lockdown be extended even further? Does South Africa’s healthcare system have the capacity to meet the surge in demand from the pandemic?
First, we consider the economic implications of a lockdown.
Covid-19 is spread by social interaction among people. To decrease the rate of infection, people work less and cut back on consumption. So both supply and demand are affected; aggregate supply decreases and people consume less as they avoid economic activity, therefore decreasing aggregate demand. The result in extreme cases, which we have reason to believe might be the case here, is economic recession. The longer a lockdown is in place, the deeper the recession.
The trade-off between the severity of recession and pandemic health consequences is driven by the relationship of economic activity to the transmission or reproductive mechanism of the virus: the virus depends on human interaction to move. Economic activity also depends on human interaction, more so than ever before in a highly interconnected global economy.
A lockdown becomes necessary when the negative externality of human interaction (increased levels of infection) are judged to be greater than the benefits therefore (economic activity).
Boston Consulting Group (BCG) recently published a study on predicted necessary lockdown periods for a selection of countries, modelled on the basis of the estimated peak in active infections, peaks in the number of new cases each day and the implementation date of a lockdown. Factors considered were the number of hospital beds available, the extent of respiratory disease in the population and the ability to manage an epidemic (which depends on factors such as political stability and government effectiveness).
Interestingly, despite South Africa being one of the few countries to implement a national lockdown early, soon after the first reported Covid-19 case (measured relative to the 10th death attributable to Covid-19), the necessary lockdown estimated by the model is longer than all countries assessed other than India, Argentina and Brazil.
BCG explains: “South Africa will require a longer lockdown to manage the epidemic due to lack of preparedness (e.g. low inpatient/bed ratio).” This is an unfortunate choice of words, given South Africa’s proactive approach in implementing such an early lockdown.
BCG’s analysis is preliminary and high-level, but nonetheless a useful indication of factors to consider in evaluating the lockdown period necessary to diminish transmission. However, any meaningful consideration of the need to extend South Africa’s lockdown must consider the country’s specific healthcare context.
World Health Organisation (WHO) data on disability-adjusted-life-years (DALYs) from 2016 (shown below) — the most recent year available — show South Africa relative to a selection of countries; some developed countries and some at similar or lower levels of development. The WHO defines DALYs like this: “One DALY can be thought of as one lost year of “healthy” life. The sum of these DALYs across the population, or the burden of disease, can be thought of as a measurement of the gap between current health status and an ideal health situation where the entire population lives to an advanced age, free of disease and disability.” In other words, more DALYs = sicker population.
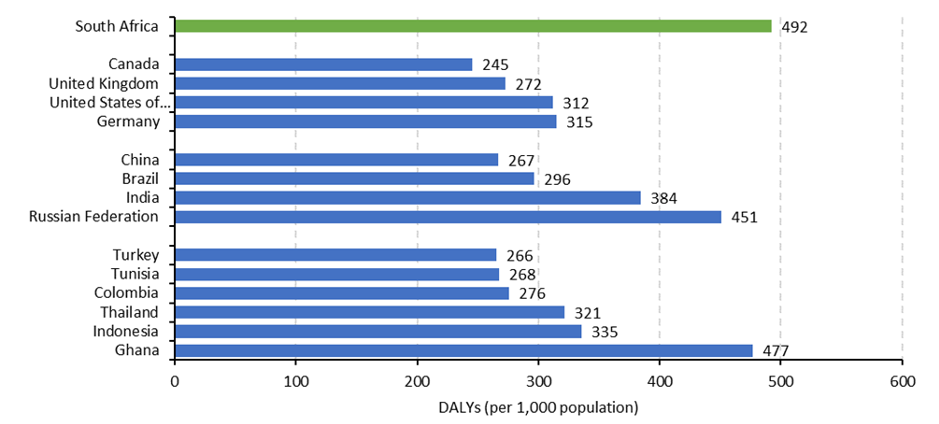
Source: WHO (2018); FTI calculations
In addition to an overall sicker population, the composition of our burden of disease (BoD) in South Africa leaves us particularly exposed. South Africa has a quadruple burden of disease. The South African Medical Research Council (SAMRC) described the quadruple BoD as “a cocktail of four colliding epidemics: (i) maternal, new-born and child health; (ii) HIV/AIDS and tuberculosis (TB); (iii) non-communicable diseases; and (iv) violence and injury”.
South Africans are sick and they’re sick from multiple causes.
We also know that, internationally, there is a social gradient to health. Health outcomes are positively correlated with income: wealthy people have better healthcare outcomes than the poor. The poor are disproportionately affected by morbidity and mortality. While this is true of overall healthcare status, it is particularly true of HIV and TB. HIV and TB prevalence is higher amongst poorer parts of the population.
In South Africa in 2018, 20.4% of people aged 15 to 49 were HIV positive, and TB incidence was 520 per 100,000 population. TB with HIV was 306 per 100,000 population. South Africa was one of eight countries comprising two-thirds of new TB infections in 2018. We also know that TB is the highest cause of death of people with HIV.
While we don’t know much about whether outcomes of Covid-19 infection are worse for people living with TB and HIV, everything we do know about these conditions (i.e. that they affect the lungs in the case of TB and that people living with HIV are immune-compromised and often have other diseases such as heart or lung conditions) is likely to mean it’s not going to go well for them.
This is particularly true of people living with HIV who are not yet virally suppressed (i.e. they are not yet on antiretroviral medication). People in this group who have high viral loads are likely to suffer a worse level of disease from Covid-19. Bottom line: the prevalence of HIV/AIDS and TB in South Africa means the impact of the pandemic will be ruthless and the poor are the most vulnerable.
From the perspective of the “direct” effect of Covid-19 on health status (i.e. the respiratory disease caused by the virus itself), if you are sick and vulnerable you will likely be affected more severely.
The capacity of the healthcare system to treat and support the infected population needing treatment will be tested. High-level estimates suggest that unless drastic measures are taken both to slow down the transmission of the virus (i.e. flatten the curve) AND immediate measures are put in place to ensure an efficient response from both the public and private sector, we run the risk of failing to adequately address the threat.
The problem is wider and bigger than that, though. If we move away from “direct” implications of dealing with Covid-19 infection and consider what the healthcare system will have to cope with, the strain on the system increases. Staying with the example of people who live with TB and HIV, let’s consider what an already overburdened healthcare system will have to contend with.
Before effective drug treatments became available for TB in the 1940s, TB was a death sentence. High mortality rates (around 70% of sufferers with sputum-smear positive pulmonary TB) were recorded. By 2017, successful treatment rates were reported among WHO member states for 85% of drug-susceptible TB. While TB is preventable and curable, adherence to treatment guidelines and treatment support are vital to ensuring successful treatment.
The WHO recommend directly observed treatment (DOT) to ensure effective treatment. DOT involves healthcare workers (or other non-family designated individuals) providing and watching patients swallow the drugs. Adherence to DOT protocol in South Africa, in the absence of a global pandemic requiring all hands on deck, is poor. Adherence to treatment protocols is likely to diminish further, worsening outcomes and increasing morbidity and mortality among TB sufferers.
The same is true for the effectiveness of antiretrovirals for people living with HIV. Successful treatment outcomes are possible and observable with strong adherence to treatment plans. Support is hugely important and necessary. In a situation where healthcare resources are diverted elsewhere, our capacity to cope with our pre-pandemic burden of disease plummets.
These are just two examples of diseases whose successful management and treatment requires adherence monitoring and patient support.
Any country characterised by high levels of diseases like TB and HIV is particularly vulnerable to the morbidity and mortality that comes directly from Covid-19 infection AND the compromised capacity of the healthcare system to service healthcare needs as a result.
The relationship between poverty and ill-health is strong. It will become even stronger if we don’t successfully control the rate at which this pandemic enters impoverished communities. It remains to be seen whether we are already too late.
Relating this back to factors determining the need for an extended lockdown period, recall that BCG cites the following factors as relevant: hospital bed capacity, prevalence of respiratory disease in the population and capacity to deal with an epidemic. These criteria suggest South Africa’s capacity to deal with an epidemic is mediocre at best.
Was a lockdown extension necessary?
Government recognises that, in the absence of effective treatment and vaccine, lifting restrictions too early may run the risk of undermining containment efforts and introducing newer, potentially higher peaks to the curve later down the line. This will place even more pressure on exhausted and exposed healthcare personnel and will place a higher number of people at risk of disease.
However, a decision to extend a lockdown must keep in mind that the relationship between poverty, morbidity and mortality is ominous. Throttling the income of people at the lower end of the wealth distribution has devastating consequences.
There are no easy answers and the country requires decisive, innovative leadership in navigating this territory. Opportunities exist; they must be matched with courageous leadership equal to the task. DM

















 Become an Insider
Become an Insider