SPECIAL REPORT
Tertiary hospital professionals sound the public healthcare alarm after severe national budget cuts

Health facilities countrywide have been adversely affected by austerity measures, which have led to vacant posts not being filled, mental health issues among healthcare workers and dire funding constraints.
Health professionals in the Western Cape’s tertiary hospitals have sounded the alarm over the impact of nationally imposed budget cuts on the delivery of health services. Dire funding constraints have led the provincial Department of Health and Wellness to restrict the filling of vacant clinical posts, while also enacting various cost-saving measures across the region.
One of these measures involves the reduction of elective surgeries.
Lydia Cairncross, head of the Department of Surgery at Groote Schuur Hospital, told Daily Maverick that the facility has had to cut about two theatre lists each day. These lists hold four or five surgical operations each, amounting to a loss of about 10 operations daily and about 100 in a month.
“These are lists which already have patients booked on them. Sometimes those patients are booked weeks or months in advance, and then we have to contact the patients and say we no longer have the list. We have to rebook them at another time and those waits get longer for individual patients,” explained Cairncross.
Over the past few years, the staff at Groote Schuur Hospital have worked hard to reduce the surgical backlogs caused by the disruption of health services during the Covid-19 pandemic. Just after the pandemic, the backlog stood at about 6,000 patients.
Since then, it has been brought down to between 3,000 and 4,000, according to Cairncross. However, as new patients are continually entering the system, the backlog only goes down when the hospital is able to increase its capacity to perform surgeries.
“If you decrease the capacity, that waiting list increases in size … I would say that every month that goes by in terms of these budget cuts at this level, we’re rolling back a month of surgical recovery … It’s really frustrating because we worked really hard to get that down,” said Cairncross.

Professor Lydia Cairncross, head of the Department of Surgery at Groote Schuur Hospital; Professor Ntobeko Ntusi, head of the Department of Medicine at Groote Schuur Hospital; and Professor Jeannette Parkes, head of the Division of Clinical and Radiation Oncology at Groote Schuur Hospital, 14 February 2024. (Photo: Shelley Christians)
The situation is affecting emergency theatre lists as well as scheduled operations, said Cairncross. “As our scheduled theatre lists decrease, it puts pressure on our emergency theatre lists because when patients wait longer, they tend to have more advanced pathology and sometimes the conditions that they have complicate.
“We often see this in the ecosystem – that as the elective lists come under pressure, it spills over into the emergency list. Things that have started off as elective become urgent.”
Cairncross gave the example of a patient with a hernia, which is a weakness in the abdominal wall that causes chronic pain and discomfort. If treated immediately, while the defect in the abdominal wall is smaller, it requires a smaller and less expensive operation, and a shorter hospital stay.
“If you leave the hernia for a very long time … then the gap in the abdominal wall becomes bigger. You need a bigger operation, a bigger mesh implant to cover the defect and often a longer hospital stay, as well as a more complicated operation. The longer you wait to intervene … [to] reverse a condition, the more complicated it is, the more health resources it uses up and the greater the complexity for the patient in terms of their recovery,” she explained.
The reduced theatre lists at Groote Schuur Hospital are also affecting waiting times for oncology patients needing surgery, according to Jeannette Parkes, head of the Division of Clinical and Radiation Oncology. In many cases, surgery is required to determine the patient’s diagnosis or stage of cancer.
“Our breast cancer patients are affected, our GIT [gastrointestinal] cancers are affected, and even our smaller lists – for example, our plastic surgery lists for our patients with very advanced skin cancers – are affected,” she said.
Compounding the problem of the reduced theatre lists is the current shortage of surgical staff at the hospital. There are positions vacant in ophthalmology, plastic surgery, general surgery, ENT and paediatric surgery, according to Cairncross.

Colorectal procedure operation being performed with the Da Vinci X1 Robot at Tygerberg Hospital on 22 February 2022 in Cape Town, South Africa. Tygerberg Hospital became the first public hospital in South Africa to perform robotic surgical procedures from 21 February to 23 February 2022. (Photo: Gallo Images / ER Lombard)
Vacant posts
Vacant posts are currently a problem across all departments and tertiary hospitals in the Western Cape. Towards the end of 2023, the severe budget cuts led to concerns that the hospitals might run out of funds to pay salaries by mid-January 2024. As a result, hospital services were de-escalated and a freeze was put on filling both clinical and non-clinical posts.
Under normal circumstances, the hospitals would begin processes to fill posts as soon as they became vacant. However, Ntobeko Ntusi, head of Medicine at Groote Schuur Hospital, reported that there were currently nearly 300 clinical and non-clinical posts that had not been filled at the Groote Schuur and Red Cross hospitals.
“Between Red Cross and Groote Schuur, we’ve made some savings from the large number of posts that were frozen. So, in January, we were allowed to fill three posts at GSH and two at Red Cross. Then, in February, we were allowed to fill four posts, one at Red Cross and three at GSH,” he said.
Groote Schuur Hospital has seen a reduction in staff across most of its divisions. The problem has been particularly acute in emergency services, where 10 of the 20 medical officer posts are vacant, said Ntusi.

Nehawu members protest outside Groote Schuur Hospital on 6 March 2023. (Photo: Gallo Images / Die Burger / Jaco Marais)
“Because it’s a constitutional mandate [that] we as a department have to provide emergency services to those who need them, we’ve actually diverted a significant amount of our resources in terms of personnel to the emergency services, which now means that if you need an appointment to be seen in many of our elective services, the waiting times are longer,” he explained.
At the beginning of February, the budget for agency nursing and overtime for nurses was frozen. This has led to a 15% nursing deficit in the surgical wards and other departments, according to Cairncross.
She added: “The nursing staff are extremely stretched in the wards and, in some cases, we are unable to get patients into beds in order to have their operations because … there are fewer beds than we had before, as you actually have to staff the beds.”
There is a large shortage of oncology nursing staff, said Parkes – a situation that will soon become a “limiting factor” for the number of chemotherapy treatments the department can provide per day.

Nurses in the isolation unit during a media briefing to discuss the first case of Covid-19 at Tygerberg Hospital in the Western Cape on 11 March 2020 in Cape Town, South Africa. (Photo: Gallo Images / Misha Jordaan)
“We’ve got a post frozen for one of our key medical officers who works in our very busy breast [cancer] clinic, which has more patients every year. And then we’ve got key radiographer planning and radiographer therapy technicians whose posts are frozen. We’ve got people acting in those positions but they’re actually not really qualified to take on that management role,” she said.
Parkes pointed out that, as more posts become vacant, the working conditions for those staff who remain become increasingly difficult. This drives more people to leave, seeking better working environments, and the number of vacant posts continues to grow – a vicious cycle.
“These are people who are on the scarce skill list of South Africa and are working in the state sector, who are basically seeing no option for themselves but to be pushed out into either the private sector or overseas, where they are actively recruiting for our very well-trained staff. So, these are not skills that we are going to easily get back,” she warned.
Sean Chetty, executive head of the Department of Anaesthesiology and Critical Care at Tygerberg Hospital, reported that the facility was also facing a large number of vacant clinical and non-clinical posts, as well as a backlog at the level of the surgical department because of the impacts of the Covid-19 pandemic and worsening budget cuts.
“We deal with the consequences of these backlogs … The impact that has for us is that now the patients who are … presented to us for surgery are sicker patients … They require more intensive care and therefore higher resources. It becomes a vicious cycle because as budget cuts … make us cut back on these non-emergency services, we see patients progressing to requiring higher resources for them to just survive,” he said.

A new Linac Machine unveiled at Tygerberg Hospital on 14 November 2023 in Cape Town, South Africa. The Linac technology will give the hospital an even better chance of improving cancer treatment outcomes for nearly 3,000 new patients. (Photo: Gallo Images / Misha Jordaan)
Health worker wellbeing
It is “extremely morally distressing” for health workers to see a patient progress to a more advanced stage of illness because they have to wait for the care they need, said Parkes. Many patients also become frustrated with health personnel when their treatment is delayed.
“We try not to make patients who we are treating with curative intent wait for their chemotherapy and radiotherapy, but we have to triage them … So, for the combined team, it’s extremely morally distressing. We have to deal with irate patients, irate families.
“There’s been very little communication about the … cutting back of services with the public, and so the public are not generally aware of the stresses and strains that are being dealt with in the hospital.
“There are a lot of mental health issues among the healthcare workers – anxiety and depression about the future, about their career paths,” said Parkes.
This sentiment was echoed by Ntusi, who said there was a “huge amount of anxiety” among medical officers and registrars about whether they would be able to advance to the next stage of their training.
“With the threat of funding cuts, there’s a large amount of jitteriness for a huge complement of our staff who no longer feel that they have job security. That is problematic. I’ve got a number of junior doctors in the last few weeks who have had to be booked off work because of admissions for acute mental health decompensation,” he said.
Ntusi added that a facility like Groote Schuur Hospital had highly specialised services that had been built up over many years.
“These budget cuts threaten to undermine the huge gains that have been made not only in procuring these important services but also in improving the quality of life of South Africans. And once you destroy something like this, it takes an incredibly long time to rebuild,” he said.
The bigger picture
The problems caused by budget cuts are being felt across the health ecosystem in the Western Cape. Cairncross, Ntusi, Chetty and Parkes are among more than 1,000 signatories of an open letter from Western Cape heads of departments, senior clinicians, nursing staff and health workers, calling on leaders in provincial and national government to reverse the budget cuts in the budget allocation for the 2024/25 financial year.
There are several factors that have contributed to the current funding crisis. In early 2023, a number of conditional grants linked to health saw a decrease in funding in the Western Cape. These grants are allocated by National Treasury via the National Department of Health.
These grant adjustments differed among provinces – in the Eastern Cape, for example, the provincial Department of Health reported that there had been no decrease in the National Tertiary Services Grant and the Human Resources and Training Grant for the province in the current financial year. However, the Eastern Cape did see a decrease in its Health Facility Revitalisation Grant and District Health Programmes Grant.
Later in 2023, a higher-than-expected wage settlement was reached between the government and public service unions. National Treasury had not budgeted for this expense. It informed provincial government departments that no new spending would be allocated for the 7.5% wage increase for public servants and they would have to fund it from their existing budgets for 2023/24.
In a joint media release issued by Western Cape Premier Alan Winde and provincial Minister of Finance and Economic Opportunities Mireille Wenger on 8 February, it was stated by Wenger that this wage agreement was “centrally negotiated without consultation, and unilaterally imposed on provinces”.
The media release noted that the Western Cape health and education sectors had since been provided with “partial funding of the wage agreement”, receiving 70% and 64.5% of what was needed, respectively. However, other departments have had to absorb the full cost of the agreement.
In the Medium-Term Budget Policy Statement released in November 2023, Treasury announced “fiscal consolidation” measures as part of a strategy to avoid a “fiscal crisis”. Spending in the current financial year was revised down by R21-billion, with further reductions expected in 2024 and 2025.
The fallout of this funding crisis is being felt in key sectors, such as health and education, across the country.
Daily Maverick asked the Western Cape Department of Health and Wellness about the amount by which the budget for tertiary hospitals had been revised down in the current financial year. However, spokesperson Dwayne Evans said that the department could only offer “broader, contextualised” responses to queries while it awaited the finalisation of the 2024/25 budget.
He added that the department was engaging in “internal consultative processes” to look at potential cost-saving measures to reduce the impacts on the health system.
“The department remains committed to providing healthcare to the citizens of the Western Cape because we know that it is our most vulnerable citizens who rely on our public healthcare system.
“We are doing everything we can to reduce the impact on our patients. No patients will be refused emergency and basic medical care and treatment. Over time, direct impact may be felt through longer waiting times at health facilities owing to fewer staff being available as well as to possible deferment of maintenance and infrastructure projects.”
Not all provincial departments of health are responding to budget constraints in the same ways.
Motalatale Modiba, spokesperson for the Gauteng Department of Health, emphasised that the department had not frozen any clinical or non-clinical posts at the province’s tertiary facilities.
“If anything, the department has ensured that priority is given to its posts so as to not negatively affect delivery,” he said. “The reprioritisation of the departmental budget is part of a normal budgeting process … All departments submit their operational plans and the proposed budget, and Treasury allocates funding accordingly.”
In an internal memorandum dated 15 February and signed by the acting head of the Gauteng Department of Health, Arnold Lesiba Malotana, it was stated that the department was facing a number of challenges regarding the approval and management of commuted overtime.
It continued: “Therefore, it has become necessary to withdraw the delegation to approve overtime applications for the upcoming 2024/25 financial year.”
When Daily Maverick contacted Modiba about the memorandum, he explained that the delegation to approve commuted overtime had been withdrawn from CEOs of hospitals and that the head of the Gauteng Department of Health would have to approve all applications for overtime.
“This decision is necessitated by challenges over the years related to the management and monitoring of the performance of overtime and consequence management which has resulted in an overexpenditure in the commuted overtime budget,” he said.
Jack Bloom, the DA shadow MEC for health in Gauteng, said the department’s decision to clamp down on overtime for doctors would lead to patients suffering.
The Eastern Cape Department of Health has continued to appoint staff in critical areas during the current financial year while still ensuring it remains within budget, according to Mkhululi Ndamase, spokesperson for the department. However, he added that health facilities had been adversely affected by austerity measures, as they had not been able to fill all vacant posts.
“Already, before the austerity measures were put in place, the department had budgetary constraints. Over the last couple of years, the department has had to walk a tightrope and do more with the little that we have,” said Ndamase.
In an internal circular dated 18 February and signed by the acting head of the Eastern Cape Department of Health, Sindiswa Gede, it was stated that the department had been faced with challenges involving newly appointed employees going unpaid from the date of their appointment “to date”.
“Officials issued appointment letters after National Treasury had imposed austerity measures and this has led to those recipients being unable to receive their salaries … Now the department has to follow a process to correct the situation,” said department spokesperson Sizwe Kupelo on the circular.
The circular stated that in future all appointment letters would need to be signed off by the Office of the Head of Department, after it had verified that all due processes had been followed.
Ntusi suggested that one of the reasons cost-cutting measures had seemed far stricter in the Western Cape than elsewhere over the past few months was that the province’s government was more “proactive” and better at taking a “long-term view” about health and other issues, whereas other provinces tended to respond more slowly to crises.
However, he criticised the failure of government officials to communicate effectively with health practitioners on the ground.
“What has been frustrating for me, particularly, is that for us who lead clinical services, we’ve been able to cultivate a very strong relationship with the leaders of health in the province, where we have a seat at the table; we can engage and contribute towards plans. And for the first time since I’ve been in this position, there’s complete silence and lack of engagement,” he said.
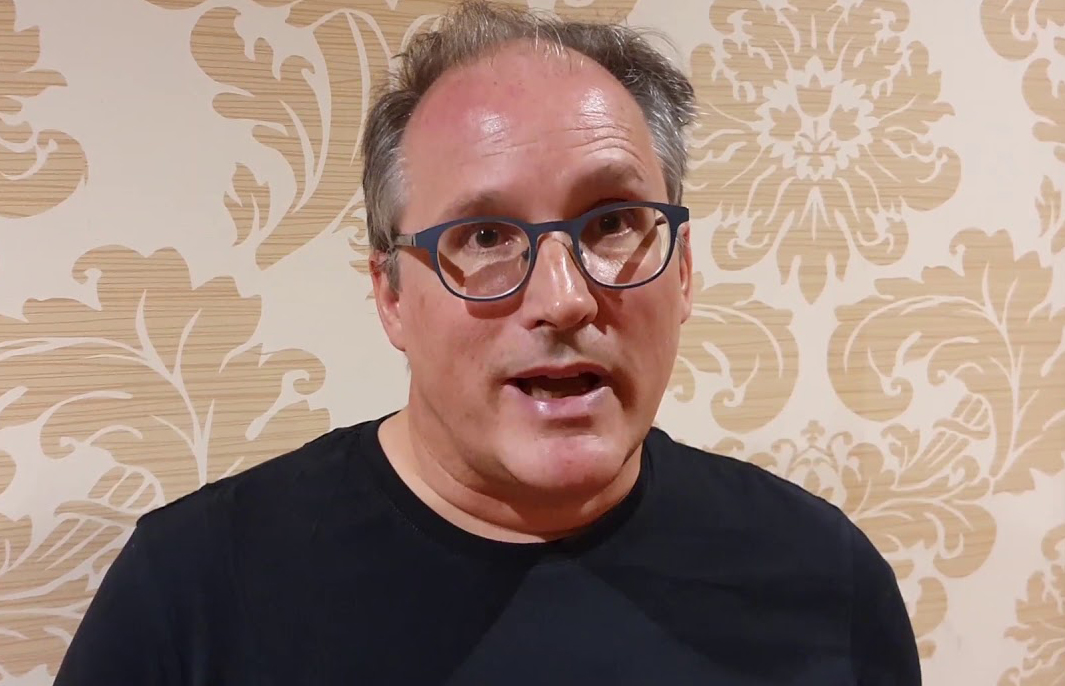
Professor Alex van den Heever, chair of Social Security Systems Administration and Management Studies at the Wits School of Governance. (Photo: YouTube)
The deeper issues
Wenger has emphasised that the fallout from nationally imposed budget cuts is “beyond the control of the provinces”, as they rely almost entirely on funding from the nationally collected tax revenue.
“This is then allocated to each of the nine provinces by the National Treasury through the Provincial Equitable Share (PES) to fund the core constitutional mandates of providing, among other things, healthcare, education and social development services,” she said.
Professor Alex van den Heever, chair of Social Security Systems Administration and Management Studies at the Wits School of Governance, raised concerns about the process for allocating the PES and conditional grants to provinces. Speaking to Daily Maverick in the lead-up to the tabling of the 2024 Budget, he said that the PES formula had criteria that bore “no relation to actual utilisation” and that were not based in science.
He compared the Western Cape and Eastern Cape, saying: “The Western Cape’s population from three years ago overtook that of the Eastern Cape. But if you look at the budget trajectories going forward, the Western Cape’s is flatlining, effectively, and the Eastern Cape’s is rising.
“This will be because of what’s going on with the [PES] weighting criteria. They’re weighting the Eastern Cape up relative to the Western Cape … despite the fact that the population’s moving to the Western Cape. This is a concern.”
According to Wenger, the latest census data were not incorporated into the PES calculations, resulting in the Western Cape, which is the third-largest province in South Africa by population, receiving the fifth-largest budget allocation. Van den Heever told Daily Maverick that the processes for determining conditional grant allocations had similar problems to those for the provincial equitable share, in that the criteria for determining the funding were not fixed or objective.
“Because there are absolutely no criteria for how these budgets are determined, there are opportunities for two things. One is a mismatch between the allocation and the actual demand for services, and the second is that the opportunities for manipulation are extremely high…
“These two sets of allocations – [PES] and the conditional grant allocations – are exposed to manipulation. They’re meant to be reviewed by the Financial and Fiscal Commission, but the commission is kind of missing in action. They don’t really do any systematic technical reviews of this kind.”
Van den Heever clarified that he couldn’t confirm that there had been political manipulation of the funding allocations for any of the provinces, but noted that the allocations did look “unusual”.
“It looks like the Western Cape is receiving an unusually low allocation relative to its population, and it’s unclear that the weights themselves are actually a valid basis for this kind of shift,” he said.
Daily Maverick sent two queries to National Treasury, one on the contents of the open letter by Western Cape health professionals and one on the issues raised by Van den Heever. The media department responded that all issues related to budgets would be dealt with during the tabling of the Budget on 21 February.
Health funds ‘slashed in real terms’ over next three years
Health Minister Dr Joe Phaahla welcomed the decision by National Treasury to “favourably consider that the current shrinking budget allocations have a negative impact on the effective functioning of the public health system in the country”.
He was responding to Finance Minister Enoch Godongwana’s 2024 Budget Speech, delivered on 21 February.
Godongwana allocated R848-billion for health over the Medium-Term Expenditure Framework, including R11.6-billion to address the 2023 wage agreement; R27.3-billion for infrastructure; and R1.4-billion for the National Health Insurance grant.
An additional R3.7-billion was allocated to the health sector for the compensation of employees for the 2024/25 financial year.
This funding is intended to address the wage bill increase and aid the recruitment of additional staff, including nurses and medical doctors, according to the Department of Health.
“Although the Budget may not address all health service delivery challenges at once, it will go a long way to enable the department to respond to the immediate and key priority needs to strengthen the health system. These include activating vacant but unfunded essential posts,” the department said.
It would soon outline plans, with timelines, for the recruitment and appointment of health workers, including recently graduated health professionals and unemployed medical doctors.
The Treatment Action Campaign, an HIV/Aids advocacy organisation, said in a statement on 22 February that, although it was “relieved” the Budget had prioritised safeguarding allocations towards health workers, the health budget was still likely to shrink in real terms over the next three years, with a R23.7-billion baseline reduction.
“In the current multiple crises of unemployment, poverty, inequality and climate change, implementing harsh fiscal consolidation measures at the expense of investment in vital public services like health is self-defeating,” it said.
“Despite concerns about the state of the country’s health facilities, the Health Facility Infrastructure grant has been cut by R3.6-billion over the next three years. It is important to note that investing in infrastructure is also an investment in job creation, something this country desperately needs,” noted the Treatment Action Campaign.
Business Day reported that, although there would be a 2.6% increase in the provincial equitable share budget, this fell below the inflation rate for the 2024 financial year.
The Western Cape’s equitable share budget increased by 2.4%, and the Gauteng and Northern Cape budgets rose by 2.8% and 3.6%, respectively. DM
This story first appeared in our weekly Daily Maverick 168 newspaper, which is available countrywide for R29.






















 Become an Insider
Become an Insider
When the tertiary hospital professionals sound the public healthcare alarm then you know it is bad. This is not just about national budget cuts but about 30 years of ANC corruption, cadre deployment and mismanagement in health care. This was brought sharper into focus when Covid hit and the ANC cadres , like our very own health minister Dr Zweli Mkhize was flagged for being involved in massive IPP corruption. This matter still goes unresolved.
Therefore, for the ANC government to try ram the NHI bill through as a bill, which should have been by referendum, shows that they are using health as a political tool in a unhumanitarian way.
Health should never be politicised. It’s too important for that. The ANC cannot even get a grip on the HIV situation in SA, which shows that SA has a cultural problem and intertwined with that, an ANC problem.
The ANC cannot implement NHI successfully with such dysfuntion.
Don’t worry folks,NHI will fix all…
How many “spokespersons” are there? More than doctors by the look of it!
It’;s not just “spokespersons”. I would wager that the ratio of administrative staff to doctors and nurses constitutes a significant factor in the degredation of health services in SA.
An ominous point in the article points to the fact that, increasingly, doctors finishing their mandatory 3-year post graduate training are simply unable to work for the state healthcare system, as registrars, house officers, etc. As the article points out, this will lead to increasing numbers of SA medical graduates to leave SA to specialise overseas. Yet another nail in the coffin of our already low doctor/patient ratio. There doesn’t appear to be any end to the ANC’s inability to govern. The effects are already protean. It will get only worse with time….
The W Cape is by far the most efficient province, better health outcomes by far….. No wonder the ANC Government is cutting budget there, notwithstanding rules and regulations regarding thiis.
Nothing to worry about folks; all will be sorted once the NHI comes into effect!
This is a mere spectre of what is on the cards for healthcare in SA. Considering the fact that SA is in essence an ineptocracy, and will likely be post the 2024 elections, I fear much worse is in store for people who need healthcare. Imagine you are planning to retire this year and what the prospect of dwindling availability of quality care will mean for you as you age. That’s a rather grim picture, I am afraid…
It is already grim for those without medical aid. For those fortunate enough to have medical aid, the situation will become grim for them, too, as private doctors flee the country, and will not be replaced by specialists, who have to train at government hospitals.