SPOTLIGHT IN-DEPTH
Concerns over treatment and care for people with schizophrenia not limited to public sector
South Africa’s shortage of public-sector psychologists and psychiatrists has made headlines several times in recent years. This has implications for the treatment of schizophrenia in that sector. But the picture in the private sector is also far from rosy, with several experts questioning the extent to which medical schemes provide cover for people with schizophrenia.
In response to a question in Parliament in 2022, Minister of Health Dr Joe Phaahla disclosed that, at the time, South Africa had only 451 public-sector psychiatrists and there were 187 psychiatric vacancies. The numbers differed drastically between provinces – the Western Cape had 99 public-sector psychiatrists and one vacancy, while the entire Eastern Cape had only two psychiatrists and 10 vacancies.
Apart from underlining large disparities between provinces, the numbers also suggest that in much of the country the public sector simply lacks the specialised staff required to provide quality treatment and care for people with potentially severe mental health conditions, such as schizophrenia. While things are generally better in the private sector, several experts contend that the treatment and care of people with schizophrenia are being undermined by insufficient coverage from medical schemes.
‘An illness of young people’
According to Dr Mvuyiso Talatala of the South African Society of Psychiatrists (Sasop), even though schizophrenia affects only about 1% of the population (rates are relatively similar between countries), it is quite severe for the people who are affected by it.
Psychiatrist Dr Eugen Allers agrees, calling it “one of the most serious psychiatric disorders we get”. Allers is in private practice and is a board member of PsychMG.
He says schizophrenia is a disease of young people, with about 90% of people with the disease first showing signs before the age of 25. “So their whole careers, their whole lives are ahead of that.”
If it’s not treated early it’s going to drain the resources because the person who’s affected will get out of work or stop working or stop studying, and they will be a burden to the state.
He says that people with schizophrenia often become psychotic, which means they hear voices, see things that aren’t there, their thought processes are confused, and they can’t distinguish between what is reality and what is not. “So, they might think they are actually Jesus Christ, or Elon Musk, or very rich or very poor. They get paranoid, they believe people want to kill them. So it’s a very serious mental illness,” he says.

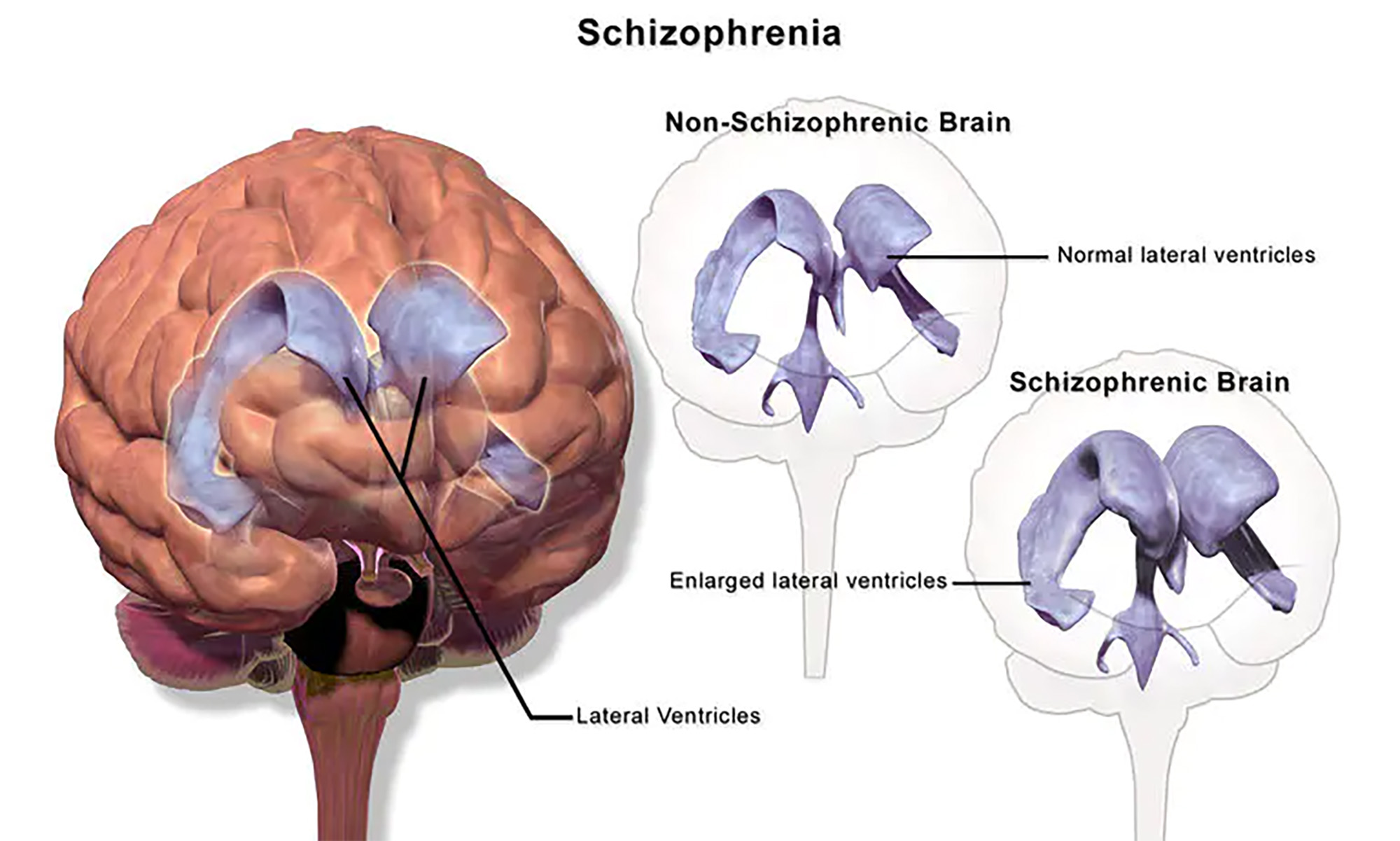
Schizophrenia is said to be a disease of young people, with around 90% of people with the disease first showing signs before the age of 25. (Image: NIH)
According to the American Psychiatric Association, when schizophrenia is active, symptoms can include delusions, hallucinations, disorganised speech, trouble with thinking and lack of motivation. However, with treatment, most symptoms will improve greatly and the likelihood of a recurrence can be diminished.
Although hearing voices and behavioural problems are among the most concerning aspects of schizophrenia, Talatala says the biggest problem is a decline in cognition, which he says occurs in the first two years. “And if you lose that cognition, you’ve lost it. It’s difficult to recover. You have to prevent it upfront.”
According to Allers, when the illness starts, people typically require medication and admission to hospital. “We usually have to admit them to hospital in that state and from there we medicate them. We also do psychotherapy to make them understand what the illness is all about. The new medications are very successful. We also have a long-acting injectable and it would last for two weeks, a month, three months or six months.” (Although he clarified that the six-month formulation is not yet available in South Africa.)
The initial first six months to a year of treatment are critical, says Allers. “The sooner you get them out of the psychosis, the better they do long-term. They can function, go to university [and] study. If you don’t do that, they become chronically disabled patients.”
Talatala also stresses this point. “If it’s not treated early it’s going to drain the resources because the person who’s affected will get out of work or stop working or stop studying, and they will be a burden to the state. They’re likely to end up in hospital care, which is more expensive.”
Schizophrenia symptoms can include delusions, hallucinations, disorganized speech, trouble with thinking, and lack of motivation. (Image: Bruce Blaus / wikimedia)
The answer, Talatala says, is treating people early. “Remember, this starts in your adolescence, late adolescence and young adulthood. If we treat these people when they’re at school, they’ll complete their studies [and there are] those who [can] start work. And we’ve seen this in our practices – where we treat patients and they continue working without anyone noticing or picking up any problems,” he says.
Private-sector problems
In the public sector, early treatment can be hard to come by if there is poor mental health screening and referral at clinics as well as a lack of beds in mental healthcare facilities and a shortage of psychiatrists. Spotlight has reported on delays at the “new” Kimberley Mental Health Hospital and problems at mental health wards in the Eastern Cape, which became the subject of a Public Service Commission investigation. Events at Tower Hospital in Fort Beaufort and the decanting of patients from the Life Esidimeni facility in Gauteng became the subject of health ombud investigations.
But appropriate early treatment also poses several challenges in the private sector.
One challenge, argues Talatala, is that regulations enacted in terms of the Medical Schemes Act on how preferred minimum benefits (PMBs) must be funded are not “crystal clear” regarding schizophrenia. (PMBs are a minimum set of benefits that all medical schemes are obliged to cover.)
With treatment, most symptoms of schizophrenia will greatly improve and the likelihood of a recurrence can be diminished. (Image: John Bill552)
“In the regulations, one needs to go and dig it out of the treatment algorithms that show some stages that should be followed in the treatment of schizophrenia,” he says. “The regulations were not written in a way that would make it easy to comply or easy for patients to fight for the funding.” As a result, he says, patients struggle to get funding to see psychiatrists or special therapists – “all the things that you need for treating schizophrenia”.
Schizophrenia should be given the same level of attention as heart attacks or strokes or any of the other severe illnesses.
The one thing that is clear enough is that, in terms of the PMBs, medical schemes are obliged to cover three weeks of a hospital stay for patients with schizophrenia. According to Allers, usually three weeks are enough, but in some instances not.
The question of what else besides those three weeks should be covered is the rub, Allers and Talatala suggest. For example, as Allers points out, appointments with psychiatrists are not covered by default. It takes six months to a year for people with schizophrenia to become really well and to get there requires intensive treatment after a hospital stay. The PMBs do not cover this (outpatient) phase of treatment and as a result patients are at risk of relapse. “Psychiatry is really more about outpatient treatment than inpatient treatment. We want to keep patients out of the hospital, not in the hospital.”
This lack of treatment and care beyond hospital admission means some private-sector patients end up being treated in the public sector. As stated in a paper published in 2022 in the journal Schizophrenia Bulletin, which Talatala co-authored: “People with schizophrenia have minimal access to care in the private sector because of this restricted funding for mental healthcare. Most people with schizophrenia are therefore treated in the public health sector.”
Talatala says the regulations for schizophrenia are poorer than those for depression. “Depression has an option of having 15 psychotherapy sessions. I’m not saying it’s adequate for depression either. And bipolar disorder has an option as well, 21 days in the hospital or 15 psychotherapy sessions,” he says. “So, depression or bipolar disorder are better covered than schizophrenia.”

Appropriate early treatment for schizophrenia also poses several challenges in the private sector. (Image: Joan Dragonfly)
He maintains that schizophrenia affects a small population, but the impacts are severe because people end up in chronic care facilities or on the streets, or in psychiatric hospitals. He argues that schizophrenia should be given the same level of attention as heart attacks or strokes or any of the other severe illnesses. “We need to treat it aggressively. To prevent heart attacks, we advertise better lifestyle care, monitoring low blood pressure, checking your blood, checking your digits, your cholesterol, and taking medication early. I think we need to have the same attitude for schizophrenia, where we look for early screening for the illness and early intervention with the medication that is effective right from the beginning,” he says.
Role of the CMS
In 2020 the Council for Medical Schemes (CMS) published a PMD benefit definition guideline for schizophrenia to, among other things, “guide the interpretation of the PMB provisions by relevant stakeholders” and to “improve clarity in respect of funding decisions by medical schemes”.
But the 2020 guideline was far from the end of the matter. Allers says they (South African Society of Psychiatrists and Psychiatry Management Group) have had numerous meetings with the CMS and particularly its clinical review committee to raise their ongoing concerns.

In terms of the PMBs, medical schemes are obliged to cover three weeks of hospitalisation for patients with schizophrenia. (Photo: Nasief Manie / Spotlight)
A circular from earlier this year suggests the CMS was listening. “Since the publication of the mental health definition guidelines, several stakeholder groups have advised regarding poor interpretation and application of the guidelines and have advised on the need for revisions. The CMS is preparing a discussion document to revise these previously published mental health benefit guidelines,” the CMS circular reads.
Once inputs in response to the circular are collated, says CMS spokesperson Stephen Monamodi, “they will be assessed and used to create an updated benefit definition guideline for the condition. This is the expected output for the 2023/24 financial year”.
CMS perspective
In response to questions from Spotlight, Monamodi confirmed that schizophrenia is a PMB condition as it is part of the Diagnostic and Treatment Pair (DTP) Code 907T and also one of the conditions included in the Chronic Disease List treatment algorithms. The specific DTP code refers to “Schizophrenic and paranoid delusional disorders”.
“The DTP treatment component as well as the treatment algorithm outline the minimum level of care that should be funded by medical schemes for any medical scheme member or beneficiary,” says Monamodi.

The lack of treatment and care beyond hospitalisation means some private-sector patients end up being treated in the public sector. (Photo: Nasief Manie / Spotlight)

Several experts question the extent to which medical schemes currently provide cover for people with schizophrenia. (Photo: Feggy Art)
“Medical schemes may also develop formularies and clinical protocols to assist in funding decisions,” he says. “The formularies must be evidence-based, cost-effective, and most importantly not result in care that is less than what is stipulated in the regulations. Therefore, in addition to hospitalisation, members’ follow-up treatment, medication, blood tests, and other tests related to schizophrenia must be paid in line with the PMB Regulations.”
According to Monamodi, the PMB regulations stipulate that PMB level of care for DTP907T is hospital-based management for up to three weeks per year. The medical treatment algorithm for schizophrenia outlines various medical treatment options that should be available when someone is treated for schizophrenia both in and out of hospital.
He says this is the minimum care that any medical scheme member or beneficiary who has schizophrenia is entitled to. However, Monamodi explains that the schemes can fund admissions for longer than three weeks or medications not on the treatment algorithm as per their protocols and formularies. DM
This article was published by Spotlight – health journalism in the public interest.




















 Become an Insider
Become an Insider
Comments - Please login in order to comment.