SPOTLIGHT
HIV vaccine research set to change focus in wake of Mosaico disappointment

Top South African HIV clinicians are setting their sights on different approaches to finding an HIV vaccine after the ‘disappointing’ news that the Mosaico trial was stopped early because the vaccine did not show any efficacy. The search for an HIV jab now seems set to shift from vaccines that induce T-cell immunity to ones that induce B-cell immunity. Adele Baleta unpacks what that means and the reasoning behind it.
Hopes for the Johnson & Johnson (J&J) Mosaico vaccine – the only HIV vaccine candidate in late-stage (Phase 3) clinical trials – were dashed with manufacturer Janssen Pharmaceuticals’ recent announcement that it lacked efficacy in preventing HIV infection. Now, top South African HIV clinicians are setting their sights on different approaches to finding an HIV vaccine.
The Mosaico study was conducted in several countries in North and South America and Europe to test the safety and efficacy of the vaccine in 3,900 cisgender men and transgender individuals who have sex with cisgender men and/or transgender individuals. Although the vaccine did not stop HIV transmission, it was found to be safe.
“We are obviously disappointed,” says Professor Linda-Gail Bekker, Desmond Tutu Health Foundation CEO and director of the Desmond Tutu HIV Centre at the University of Cape Town. “But with the decades-long search for an elusive vaccine to prevent HIV, those of us in the HIV vaccine field have developed resilience. So, it’s back to the drawing board. Our mantra is not to give up, but to go back to the bench to figure it out more and give it another go. We can’t give up on this. It’s too important,” she says.
The “mosaic” vaccine incorporates genetic material from HIV strains from around the world, and was trying to induce non-neutralising antibodies, those that don’t work on their own to stop the virus, but work with the cellular immune response (T-cells) to try to contain the virus, and eliminate it.
The vaccine applied the same antigen delivery system (or viral vector platform) – a common cold virus called adenovirus 26 – that was used in J&J’s Covid-19 vaccine.

Professor Linda-Gail Bekker. (Photo: Facebook)
The Mosaico findings are the latest in a series of disappointments.
In 2021, a Phase 2b trial (called Imbokodo, or HVTN 705) of a similar vaccine tested in cisgender women in five southern African countries was prematurely stopped due to a lack of efficacy in preventing HIV infection. In 2020, an HIV vaccine (HVTN 702) trial in more than 4,500 HIV-negative 18- to 35-year-olds across 14 sites in South Africa was also halted. It too proved to be ineffective in preventing HIV transmission.
Professor Glenda Gray, president of the South African Medical Research Council and co-principal investigator of the National Institutes of Health-funded HIV Vaccine Trials Network (HVTN), says the Mosaico and Imbokodo trials have shown that the incidence of HIV is “off the charts” and non-neutralising antibodies against HIV infection have not worked.
New vaccine approaches
Both Bekker and Gray say that with the experience of Covid-19 vaccine design, the strategy for HIV is now to find immunogens and technology platforms that induce broadly neutralising antibodies rather than non-neutralising antibodies.
“The messenger RNA (mRNA) platform can help us as it induces potent neutralising antibodies,” says Gray.
The HIV clinicians see the mRNA platform as promising because they can iterate very quickly – meaning they can change or modify their approach – while using it. The ability to modify approaches is essential given the ability of the virus to hide and mutate rapidly.
Read in Daily Maverick: “Anti-HIV jab could be in SA clinics by August 2023 — if the price is right”
The discovery of Covid-19 vaccines in under two years compared with the decades-long search for an HIV vaccine without success is partly due to the first-time use of the mRNA vaccine platform and the ease with which researchers were able to target the SARS-CoV-2 spike protein. One reason HIV vaccines are harder to develop is that there isn’t a clear target on the virus like that spike protein.
The Pfizer/BioNTech Covid-19 jab used in South Africa is an mRNA vaccine.

The discovery of Covid-19 vaccines in under two years compared with the decades-long search for an HIV vaccine without success is partly due to the first-time use of the mRNA vaccine platform. (Photo: iStock)
Bekker, co-principal investigator with Gray for the J&J Covid-19 Ad26 vaccine (Sisonke) trial in South Africa, says: “We got to know the Ad26 platform during Covid-19. It was familiar, but it was not meant to be for HIV.”
She explains there are two broad ways in which the immune system tackles pathogens – via B-cells and antibodies, and via T-cells. “When we’ve looked at HIV vaccines in the past, we leaned more towards a T-cell type response versus an antibody (B-cell) response.”
The Covid-19 Ad26 J&J vaccine “really brings its magic about through T-cell activity, whereas the mRNA Covid-19 vaccines give more impetus to antibodies (B-cells)”, Bekker says. The impact on severe disease, on making sure that the infection was not as serious, was around T-cell activity.
Read in Daily Maverick: “HIV treatment in South Africa is changing — here are seven things you need to know”
The hope was that even if the vaccine did not stop infection, the infection would be less severe, the viral load lower – meaning that the initiation of ARV treatment could come later.
“We have come through an era and realised that these vaccines did not play out. We really want to stop infection if we can, and this means we are going to need an antibody, which is a B-cell type of response,” she says.
Monoclonal antibodies
Researchers are now trying two different ways of inducing broadly neutralising antibodies to fight HIV. The one is to infuse them directly, similar to pre-exposure prophylaxis, in that it works for a time only, but it’s hoped it will last longer than the currently available PrEP. “The idea is that you infuse an antibody which, when it sees the pathogen, immediately cling-wraps it, packages it up, and spits it out of the body. It gets rid of the pathogen right there and then. So it really does prevent infection. It doesn’t even allow the infection to take a foothold,” says Bekker.
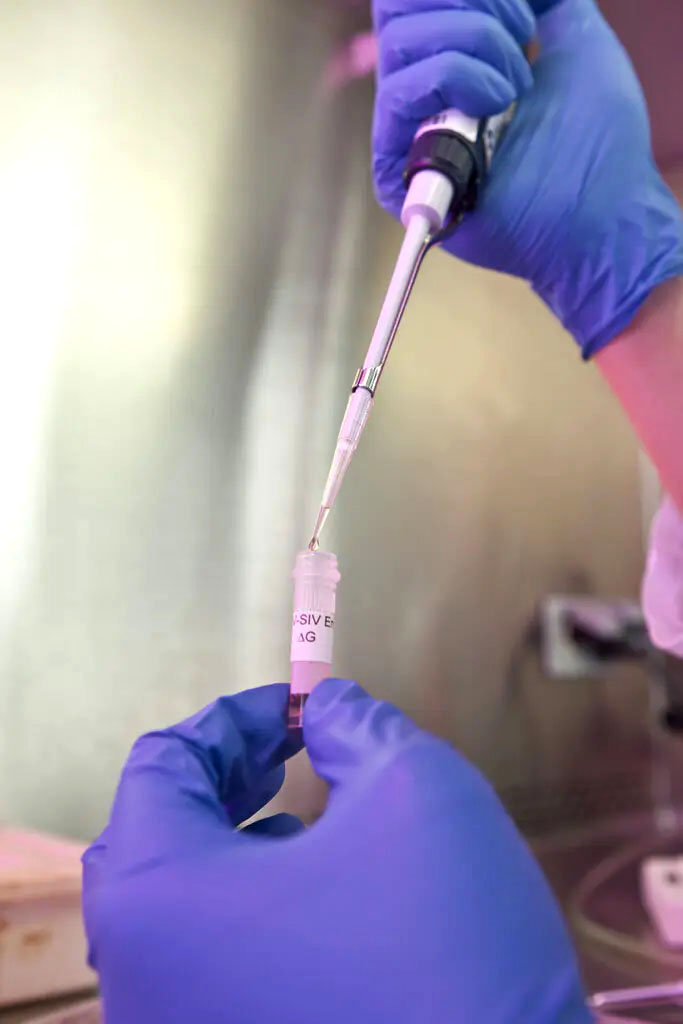
Experts say, building on Covid-19 experiences, the strategy for HIV is now to find immunogens and technology platforms that induce broadly neutralising antibodies rather than non-neutralising antibodies. (Photo: Frederic Courbet / IAVI / Spotlight)
There has been some evidence of this approach with the antibody-mediated prevention Phase 2b studies reported in 2021. In those studies, a single monoclonal antibody known as VRC01 was infused into women who have sex with men in South Africa, while the second trial was among HIV-uninfected men and transgender persons who have sex with men in the Americas.
“We found that as long as the HIV that was invading the body or attempting to infect the body was aligned to the VRC01, [and] as long as they were matched to each other, so the antibody was designed to cling-wrap the HIV that was invading, it was very effective at stopping the HIV,” says Bekker.
Visit Daily Maverick’s home page for more news, analysis and investigations
However, HIV is genetically extremely diverse. There are more than 60 dominant strains and if the virus looked different from the broadly neutralising antibody, it had no impact.
“For HIV, one monoclonal antibody is not enough. We need to invest in more panel antibody research. We need to fast-track monoclonal antibody cocktail efficacy studies to demonstrate their utility,” says Gray.
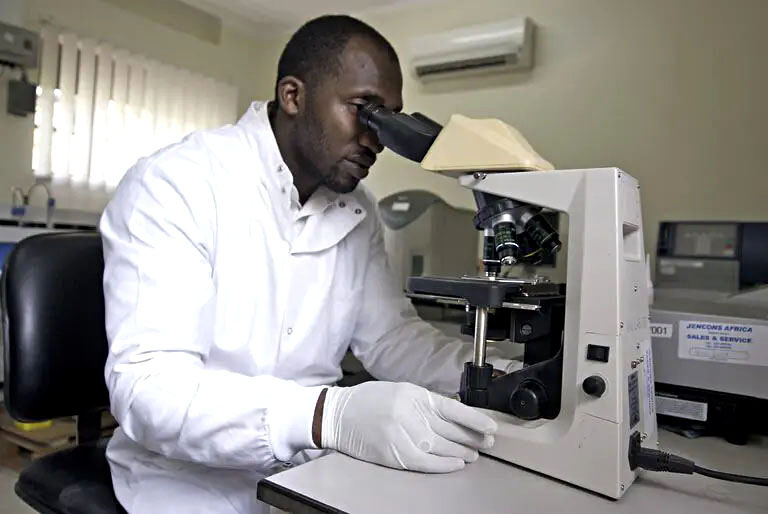
The search for an HIV jab now seems set to shift from vaccines that induce T-cell immunity to ones that induce B-cell immunity. (Photo: Charlotte Raymond Photography / IAVI / Spotlight)
Researchers are now designing studies using three monoclonal antibodies. Bekker says there are challenges to infusing monoclonal antibodies. “As we saw during Covid-19, they are expensive, so how do we make them cheaper? How do we make them last longer and how do we make them subcutaneous (under the skin) rather than infusions? Nobody wants to come to hospital to get prevention.”
Active vaccination
The second way to induce broadly neutralising antibodies, Gray says, is to “mimic” these antibodies with active vaccination. “We need to find a way to train the host, the human, to make these broadly neutralising antibodies, which cling-wrap pathogens and get rid of them straight away. That’s the impression we are now getting. That’s the route we need to go.”
Bekker says there is a strategy to “shepherd” the immune system in that direction and what researchers are currently imagining through a series of experimental medicine trials is to “vaccinate then re-vaccinate and re-vaccinate, to coax human immunity to work towards that broadly neutralising antibody – to train the immune system to go in a particular direction”.
Read in Daily Maverick: “Six graphs that tell the HIV story in South Africa”
The first of these vaccines had been tested in humans in an early-stage clinical trial.
Gray says that even though we have not found a vaccine to prevent HIV, the spin-off for South Africa and the world “has been great in terms of crystallography, understanding virus envelopes and having platforms to insert the genetic structure of new emerging pathogens”.
Not continuing to invest in HIV vaccine design would be at the world’s “peril” because the milestones reached in HIV research were usually “translatable”. For this reason, HIV research needed to be encouraged, as well as young scientists. There is a disturbing trend of young scientists migrating from infectious diseases to cancer and other non-communicable diseases, Gray adds.
“We are losing momentum in terms of scientific career development. We have to keep the field open for discovery. We need to continue to do this even though we have setbacks. We should see this as a global scientific challenge.
“We need a vaccine. We need vaccine discovery, we need continued investments at a global level. HIV happens in poor people and in key populations. And sometimes poor people and key populations are not the priority of the rich,” Gray says. DM/MC
This article was published by Spotlight – health journalism in the public interest.






















 Become an Insider
Become an Insider
Comments - Please login in order to comment.