MAVERICK CITIZEN
Ritshidze Report: Public healthcare in the Eastern Cape has deteriorated significantly since outbreak of Covid-19

Staff attitudes, long waiting times and dire personnel shortages have seen public healthcare in the Eastern Cape, specifically for people living with HIV, regress significantly since the outbreak of the Covid-19 pandemic, a report by Ritshidze has found.
Covid-19 had a significant negative impact on healthcare services in the Eastern Cape, according to a research report released on Thursday, with many people living with HIV bearing the brunt of bad staff attitudes, personnel shortages and long waiting times at clinics.
The report was released by Ritshidze, a project implemented by organisations representing people living with HIV including the Treatment Action Campaign, the National Association of People Living with HIV, the Positive Action Campaign, the Positive Women’s Network and the South African Network of Religious Leaders Living with and affected by HIV/AIDS (SANERELA+), in alliance with Health Global Access Project, the Foundation for AIDS Research and Georgetown University’s O’Neill Institute for National and Global Health Law.
It was presented to the Eastern Cape health department in Mdantsane.
Bad staff attitude was highlighted as a major barrier to seeking help at public health facilities.
“Over and over Ritshidze is hearing complaints about poor staff attitudes and unprofessional conduct by nurses. Only 64% of patients we interviewed thought that clinic staff were always friendly and professional and people living with HIV at 25 facilities monitored complained of being shouted at if they missed an appointment,” Bellinda Setshogelo, a Ritshidze project officer, said.

Maluti Clinic, Eastern Cape. (Photo: Noluvo Gasmeni)
“While nurses may be burdened with their own challenges, and are in some cases overworked and overwhelmed by their patient load and shortage of support, their attitudes and work behaviour remain one of the easiest targets to shift if the Department of Health can commit to bringing their employees to order. These problems seem insurmountable but there are targets that the province can and must improve on,” she added.
Akona Ntsaluba, a Ritshidze key populations organiser, said: “Another woman, who is trans, explained to me how the staff at the clinic judge her. One nurse referred to her as ‘another one of those who don’t know what they are’ to her colleagues. Humiliated, she left the clinic without getting any medication or any further help. She said she felt that there was no point in complaining as they just make fun of you if you are LGBTQI. Even the suggestion box is useless. She has vowed never to return to Thanduxolo Clinic because of her traumatising experience there.”
“Improving the quality of services provided in public clinics is vital to ensuring enough people are accessing HIV and TB prevention services, are getting tested, and are starting and staying on treatment. It is key to achieving the Unaids new scaled-up 95-95-95 targets that now aim for 95% of people living with HIV knowing their HIV status; 95% of people who know their status on treatment; and 95% of people on treatment to have suppressed viral loads,” the report states.
The report also highlighted the dire staff shortages in many facilities, saying these should be addressed as a matter of urgency.
Nomangesi Clinic, Eastern Cape. (Photo: Rian Horn)
“Ensuring that 80% of vacancies at facilities are filled by March 2022 must be a priority in this province. The majority (89%) of facility managers do not have enough clinical and non-clinical staff at the facility to meet the needs of patients. Data from patients are closely aligned: just 29% of patients interviewed report that there are always enough staff at the facility.”
Staffing was one of the issues that must be addressed for the province to significantly improve its health statistics and meet the new Unaids targets.
According to Health Department statistics, 91% of people living with
HIV know their status, but only 72% of those people are on HIV treatment and only 88% of this smaller group are virally suppressed.
“This translates to just 66% of all people living with HIV receiving ARVs in the province and only 58% of all people living with HIV being virally suppressed,” the report states. “The failure to make sufficient progress towards the 95-95-95 targets, most especially keeping enough people on treatment, can be directly linked back to the crisis in our clinics in the Eastern Cape.”
In 2019, in a circular the Department of Health proposed a series of policy changes designed to remove barriers to care and support accountability of healthcare workers, but Ritshidze researchers found that two years later, this directive has not been enacted by many facilities.
The report further states that since the outbreak of coronavirus infections in the country there was a decline in the overall number of visits to health facilities in the Eastern Cape, and fewer HIV tests were carried out in the province. When looking at statistics for tuberculosis there is a similar trend, with a decline in the number of GeneXpert tests carried out.

Greenfields Clinic, Eastern Cape. (Photo: Siphosethu Ndebe)
“Fewer people getting tested for HIV and TB will lead to an increase in the number of people with undiagnosed HIV or TB, and add to those not yet initiated on treatment,” it said.
Researchers interviewing patients at clinics in the province found a few significant trends at all clinics that were constituting a significant barrier for many patients in seeking healthcare. They included:
- Longer waiting times;
- Fewer staff members working than usual;
- Increased stockouts; and
- A lack of personal protective equipment and a lack of safety precautions at some facilities, including no physical distancing, a lack of water/soap or sanitiser, and at times screening protocols not being followed.
“A reduction in the overall provincial health budget due to costs associated with the Covid-19 pandemic – together with budget cuts from Pepfar and an end to additional surge funding that aimed to maximise progress towards the 95-95-95 targets – is only worsening this crisis,” the report added.
Significant staff shortages are also “undermining the quality of services provided at clinics”, researchers found. “Ensuring access to quality healthcare services and ensuring everyone living with HIV and TB gets access to medicines and care depends mainly on having enough qualified and committed staff. These shortages, including a high number of vacancies, lead to longer waiting times and increased pressure on the few staff in place.”
Most of the vacancies at clinics are for professional nurses, enrolled nurses, cleaners, doctors, enrolled nurse assistants and assistant pharmacists, according to Ritshidze researchers.
“What is clear is that both facility managers and patients agree – there is a major gap between the staffing needed to ensure high-quality services and the staff present each day in the clinics in much of the province, compounded by Covid-19 and unfilled posts,” the report added.
The report also highlighted the importance of community health workers in the fight against HIV/AIDS and TB as well as Covid-19, since they play a huge role in defaulter tracing (95% of sites), TB contact tracing (80% of sites), HIV testing and counselling (61% of sites) and treatment literacy (56% of sites).
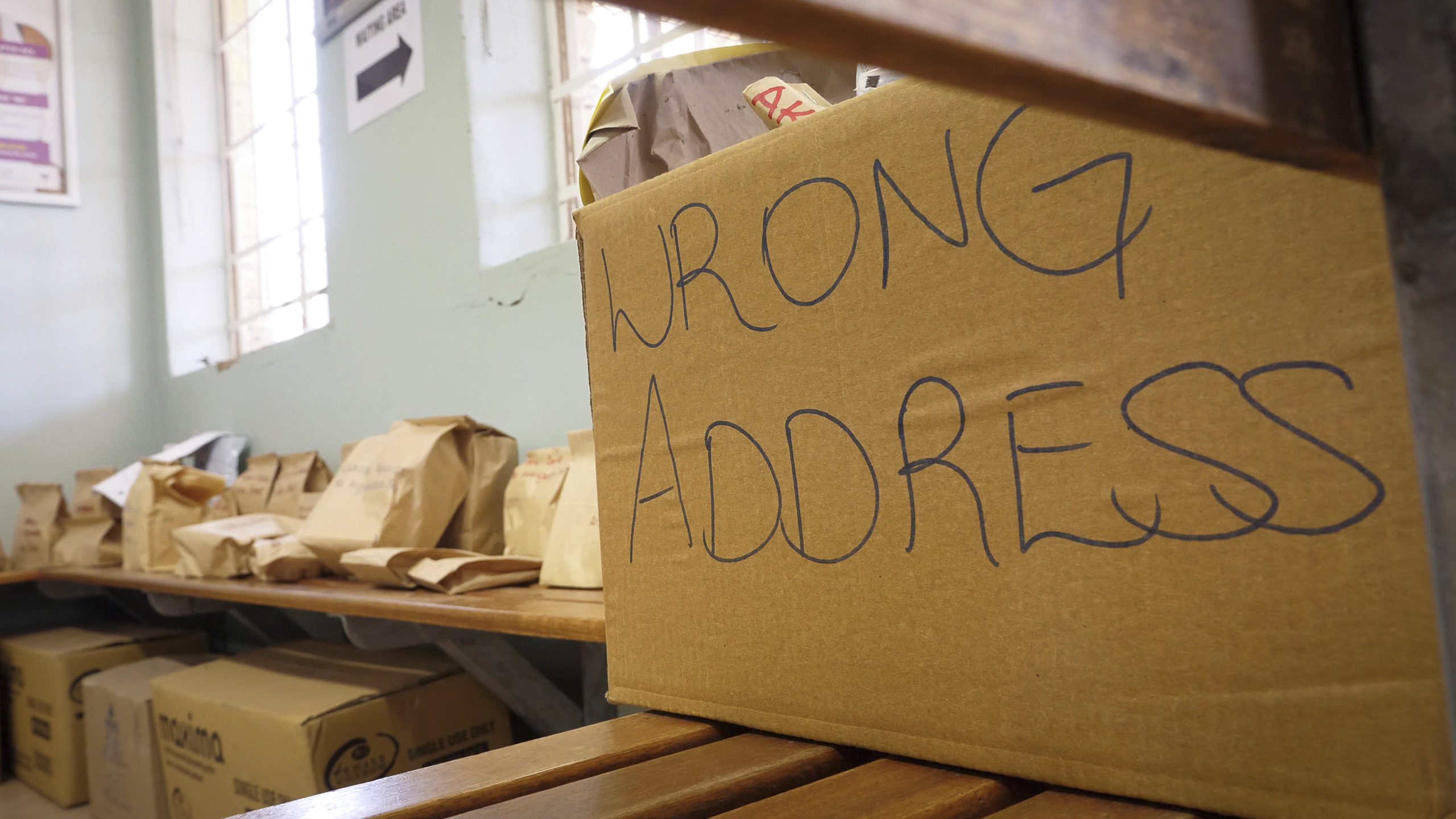
Yet, facility managers report that many community health workers do not have transport available to do their jobs, do not have enough phones, and fear for their safety. Many managers also said tracing patients was made very difficult by people giving them the wrong numbers and addresses.

Mount Frere Gateway Clinic, Eastern Cape. (Photo: Noluvo Gasmeni)
“Long waiting times are a major challenge in the Eastern Cape, where public healthcare users often spend hours at each visit to the clinic. This simply does not work well for most people – particularly working people and those in school. Having people living with HIV spend an extended time at a clinic, simply to collect ART refills, increases the risk of that person disengaging from care. In the Eastern Cape, public healthcare users reported that they spent an average of 4.41 hours waiting in the facility (including time before the facility opens) as well as an average of 4.31 hours waiting after the facility opens. The average was seven hours or more at three facilities, six or more hours at six facilities, five hours or more at 16 facilities, and four hours or more at 29 facilities. This is a very long time to spend at a facility in which patients are usually only seen for a very short consultation.”
‘Severe overcrowding’
“Through our community-led monitoring we hear many stories from people living with HIV, key populations and other people using public clinics about the challenges they face in accessing healthcare. It is these challenges that make it hard for someone to test for HIV, access HIV prevention options, or even to stay on their HIV treatment once they have started. Today’s meeting is giving community members the chance to tell these stories directly to those in power,” Anele Yawa, from the Treatment Action Campaign, said.
“Severe overcrowding and clinics that are too small to service their growing number of patients are just the start of problems for the Eastern Cape – a province that remains one of the poorest in the country. Added to this are challenges of improving road access and general amenities to some of the most remote parts of South Africa. It makes the problem of attracting and retaining nurses and doctors to these far-flung regions a tall ask. We can see this in Ritshidze’s data where 133 unfilled vacancies have been reported across 28 of the facilities monitored,” Ndiphiwe Bekwaphi, a Ritshidze district organiser from the TAC, added.
Ritshidze project officer from SANERELA+, Simphiwe Xaba, added: “Two solutions include getting more people living with HIV out of the clinic and into external pick-up points, that are quicker and friendlier ways to collect ARV refills, as well extending ARV refills to three- or six-month supply. Together these can reduce the burden on clinics, ease congestion and reduce unnecessary interactions between patients and clinic staff. Yet, currently only 15% of people living with HIV that we spoke to are getting three-months’ supply and 3% are getting a six-month supply, compared to 22% who received a six-month supply and 53% receiving a three- to five-months’ supply in other countries.”
Mandisa Ndinisa, a Ritshidze community monitor from the Positive Women’s Network, added: “One woman explained to me how, after being retrenched at short notice, she didn’t have enough time to go to the clinic to ask for a transfer letter. But when she got back home and went to the Matatiele Clinic, they said they wouldn’t help her because she couldn’t show them a transfer letter – even though they knew her from before she went to Joburg.
“It means she hasn’t returned to the clinic in months and as a result she has defaulted on treatment. It’s been nine months since she was last on her ARVs. She knows that returning for treatment after an extended break will just invite being shouted at and being given a dressing-down – in front of everyone. She says it’s too much, she doesn’t want to go back.”

Nomzano Community Health Centre (CHC), Eastern Cape. (Photo: Rian Horn)
Olona Soyamba, a Ritshidze community monitor from the National Association of People Living with HIV, said: “One man told me he has not received his viral load test results, even though he took the test a year ago. They keep telling him they will add the results to his file, but they cannot find them. This does not sit well with him because he doesn’t know if the treatment is working or not. He didn’t know the name of his treatment either, just that he should take one pill at night – showing that treatment literacy is not happening at the clinic.”
The newly appointed head of the Eastern Cape health department, Dr Rolene Wagner, who started on 1 August, also identified getting programmes for HIV, TB, maternal care, women and child health and chronic disease management back on track, following the onslaught of the Covid-19 pandemic, among her most pressing priorities.
“We will need to reconnect with our patients and communities to ensure they are compliant with treatment; and to screen for early detection and management of these conditions,” she said at the time of her appointment.
Earlier in September, Wagner said the province was using a web-based stock visibility system to monitor stock levels of personal protective equipment from 786 clinics and 90 hospitals. The current stock status in the province is 85.7%. DM/MC





















 Become an Insider
Become an Insider
Doesn’t anyone maintain anything in this country anymore?
Desperate situation. Reading through this article we read of many issues and problems which may not be only in the Eastern Cape. Doesn’t the Department of Health have regularly updated metrics where progress on issues are reported from all Provinces. “In 2019, in a circular the Department of Health proposed a series of policy changes designed to remove barriers to care and support accountability of healthcare workers, but Ritshidze researchers found that two years later, this directive has not been enacted by many facilities.” This is absolutely disgusting that no or little follow up has been done.