SPOTLIGHT
Why broadly neutralising antibodies might be the next big thing in HIV
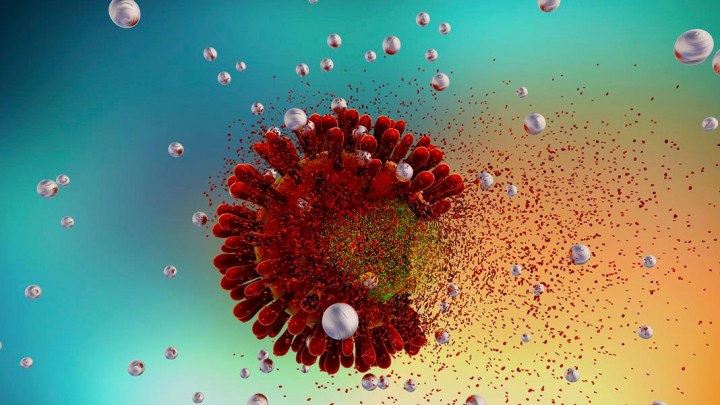
We know antiretroviral therapy can prevent HIV infection, but can natural biological substances do the same? The results of a recent scientific trial have answered this question: Yes, using broadly neutralising antibodies. But what are broadly neutralising antibodies? How do they work? And when will the average person get access to them? Spotlight breaks down the science.
Results of a “proof of concept” study presented at the virtual 4th Research for HIV Prevention Conference last week showed that one particular broadly neutralising monoclonal antibody (bNab) – called VRC01 – prevented HIV infection in more than 70% of people exposed to strains of HIV sensitive to this particular bNab.
The study, which “was really probably one of the more complicated studies ever done in the [HIV] prevention field” according to Professor Larry Corey, former president of the Fred Hutchinson Cancer Research Centre, enrolled 4,600 people globally, predominantly women living in sub-Saharan Africa as well as men who have sex with men and transgender persons in the Americas.
Speaking at a press conference, Corey, who was the principal investigator for AMP – the Antibody Mediated Prevention Trial – explained that every two months, over a 20-month period, participants received intravenous infusions of this antibody. Although it did not protect against the majority of HIV strains (only 30% of strains were sensitive to the antibody), this is the first time in history that it has been shown that a natural substance, produced in a human body, can prevent HIV infection.
Of course, the bNabs used in the study were manufactured in a laboratory, but unlike pharmaceutical drugs, they are naturally occurring substances.
But what is a bNab and what does all this mean for the future of HIV prevention?
“When a person is infected with HIV, this elicits an immune response in the person in a part of the immune system called antibodies,” says Professor Linda-Gail Bekker, Director of the Desmond Tutu HIV Centre at the University of Cape Town.
She explains that these antibodies, which are types of proteins, come in two types. “With what we call neutralising antibodies, essentially what happens is this kind of antibody envelopes the virus, something like cling wrap. It packages it and then it is discarded from the body – it makes a lunch-wrap out of it and gets rid of it,” she said.
The other kind is called a non-neutralising antibody which, she says, “does work but aren’t as explicitly effective”.
“Broadly” neutralising antibodies are neutralising antibodies that “neutralise a larger number of HIV variants – a broader range” explains Mitchell Warren, the executive director of the United States-based advocacy organisation, Avac.
The “broad” aspect is vital because HIV is a wily virus that mutates constantly. There are very many variants of HIV, which is why the need for a broadly neutralising antibody or a combination of bNabs is important.
“In some diseases, the antibodies, the human immune system’s response, are able to fight off a virus by themselves. But with HIV, the virus always wins the fight. But these antibodies get created, and the scientific work being done now is finding these bNabs and understanding which ones have the most effect,” he says.
In a press release, the International Aids Society (IAS) notes that the AMP trial builds “off of traditional notions of vaccination, in which a vaccine primes the immune system to make antibodies that can neutralise an infectious agent such as HIV” but “instead of priming recipients to create antibodies, the AMP study infused participants” with the VRC01 antibody.
Viable and safe
The AMP study, which was randomised, controlled and double-blinded, showed 74% protection for an HIV variant that accounted for 30% of the variants to which study participants were exposed.
This might appear like a small victory, but it is very significant to the field. For the first time, using bNabs for HIV prevention has been found to be both viable and safe.
Over the course of the study, says Corey, “we gave 46,000 infusions, frankly without any incidents” in other words without any serious side-effects.
“Like most innovative research studies, AMP produced complex results that also raise important new questions for researchers,” says Roger Tatoud, from the International Aids Society (IAS) in an IAS press release. “Moving forward, the field must consider the dual challenges of developing cocktails of antibodies that are both more broadly effective and more easily and practically delivered, while remaining affordable and accessible.”
Just like with ARV therapy, where it was found that one drug was not potent enough to suppress the virus – a combination of three drugs are generally used today – it is thought that with bNabs a “cocktail” of a number of candidates will be needed to provide wide protection from the vast variety of variants, according to Bekker.
Picking winners
The second important outcome of the AMP study, according to Warren, is the development of an assay, or laboratory test, “that can help us more rapidly select which combination could be used in larger trials of the future”.
“The good news is the field has developed a large cadre of monoclonal antibodies. We’ve actually developed a tool that allows us to rapidly assess if one antibody is better than another, which ones are more potent and more likely to succeed. Yes, it would have been nice if the virus was more susceptible to VRC01, but there are many other antibodies in the toolkit that show promise for this modality of prevention,” says Corey.
This is vital, says Warren, because “we can’t test all possible combinations in $100-million trials so we need a way to select which ones to even try in larger trials”.
“The AMP trial’s greatest gift to the field is this assay lab test that identifies which ones stand the best chance of working against the largest number of viral strains,” he says.
Improving real-world viability
There are other issues that remain unanswered with the viability of using bNabs in future prevention efforts.
Bekker says the route of administration would need to change for this option to become feasible, for example, in the form of subcutaneous injections (like those used for insulin by diabetics) either administered by patients themselves or healthcare workers.
Another feasibility issue is timing. Corey says that studies are under way to see if bNab infusions every four or six months (as opposed to the two months in the AMP study ) will be just as powerful at preventing infection. This is especially important to countries like South Africa, where many do not have the means to travel to distant clinics often.
Where does bNabs fit in our HIV prevention toolkit?
But why invest in bNabs if we already have antiretroviral drugs to prevent HIV – termed pre-exposure prophylaxis – that are close to 100% effective if taken correctly, especially since the costs of manufacturing antibodies remain relatively high? In other words, where would bNabs fit in our HIV prevention toolkit?
“That’s an important question,” says Bekker. “There are people who – for whatever reason – can’t take ARVs. These are natural and based on things our own bodies make. There might be a lot of people who don’t do pharmaceuticals or won’t take chemicals, and for these people bNabs are ideal.”
But, she says, the “big question on everybody’s mind is how much is this going to cost”.
“To be cost-effective they would have to become a lot cheaper than they currently are to make. Already we have fantastic monoclonal antibodies used in cancer and rheumatology, but people in this country don’t have access to them because they are unaffordable. We have to change that paradigm,” says Bekker.
Warren is more optimistic that costs will fall much as they did with ARVS, which, when they first came to market, were unaffordable to much of the world’s population, but with advocacy and political pressure they were eventually sold at a cost that countries like our own could afford.
“The cost of antibodies are already dropping, the use of antibodies in medicine is increasing, and the manufacturing and technologies associated with their development are advancing. I think they will be economically feasible for HIV prevention if they are proven to have high efficacy,” says Warren.
Role in cure research
Another exciting idea being investigated by scientists is whether bNabs might play a role in curing HIV infection.
“There are studies under way starting to look at ARVs and monoclonal antibodies to look at complete eradication of HIV in someone already infected. We don’t yet have any successful results on this, but there are promising results in animal studies,” says Bekker.
She says that there is even more “good news” in that “there is already a lot of work going on in the bNab space”.
“There is a pipeline of very exciting bNabs – some already in phase one and two trials. I would imagine these results from the AMP study would give the green light to actively start development and move things further down the phases and that we might begin to see activity in this area right away.”
But what does that mean to the average person? How long will we have to wait before we see bNabs in our local clinics?
“Well, how long is a piece of string?” asks Bekker.
“With Covid-19, a new disease arrived in January, and by November we were able to inject a monoclonal antibody into the president of the United States’ arm. This took exactly one year and shows what can be done when people are geared up and doing everything they can to make it work,” she says.
“With bNabs and HIV, it’s hard to predict. If everyone got behind this, we could do it in no time at all. But the problem we see in HIV is that it doesn’t have the private sector backing Covid-19 had. We’ve learnt from the Covid space what an amazing difference it makes when industry, academia, political leaders and everybody gets behind a problem. When this happens, we can do extraordinary things. We need the world to embrace what can be achieved in HIV again.” DM/MC



















 Become an Insider
Become an Insider
Comments - Please login in order to comment.