SPOTLIGHT
Key populations frustrated by “uncaring, disrespectful and cruel treatment” in public health system

Nthusang Lefafa looks at the latest Ritshidze report for key populations and speaks to some public healthcare experts about possible solutions to challenges facing those marginalised groups who carry a high burden of the HIV pandemic.
Many people at high risk of contracting HIV or already living with HIV continue to face uncaring, disrespectful, cruel and even abusive treatment when visiting clinics and community healthcare centres, according to the third edition of the Ritshidze State of Healthcare for Key Populations report. It also found that because of discrimination and privacy violations, some patients stop taking their treatment or leave the clinics without the services they need.
Key Populations – including sex workers, gay men, transgender people, people who inject drugs and prisoners – accounted for 70% of new HIV infections around the world in 2021, according to the US Agency for International Development. According to South Africa’s fifth National Strategic Plan for HIV, TB and STIs 2023-2028, key populations have the highest prevalence and incidence of HIV in the country for a number of reasons, including inadequate efforts to reach these people, stigma and discrimination.
HIV prevalence in women sex workers was about 59% in South Africa in 2022 and 30% among men who have sex with men, according to the most recent estimates from Thembisa, the leading mathematical model of HIV in South Africa.
For this year’s Ritshidze report, 13,832 people were surveyed, including 2,612 gay, bisexual and other men who have sex with men, 6,097 people who use drugs, 3,700 sex workers and 1,423 transgender people. The data shows that 75% of people in key populations use public clinics. Very few people said facility staff were nice to them and privacy violations are extremely common.
A cursory Spotlight assessment found that some of Ritshidze’s latest findings are worse than those it recorded in 2021 and 2022. Though such year-on-year comparisons should not be overinterpreted – the survey sample and some survey questions changed year on year and Ritshidze does not conduct all the statistical analysis one would see in academic publications – the picture is nevertheless grim and based on real-world reporting by affected people and therefore worth taking seriously.
Ritshidze is a community-lead clinic monitoring project implemented by several organisations representing people living with HIV, including the Treatment Action Campaign and National Association of People Living with HIV.
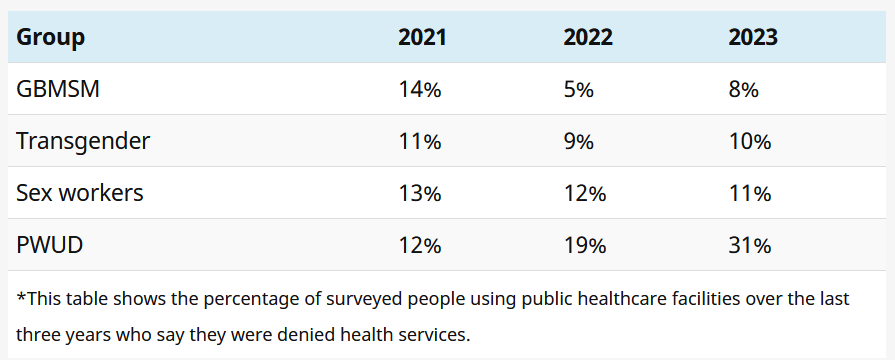
Access to health services
Regarding members of key populations being denied access to healthcare, the Ritshidze data generally does not show any clear trends over the past three years – although its reports provide compelling evidence that some people, probably in the region of 10% of those in key populations, are being denied service. The one group for whom things appear to have become worse over the past three years is people who use drugs.
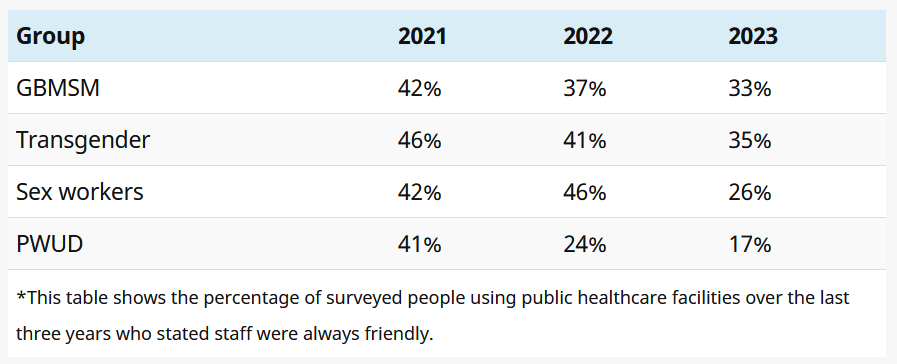
Friendly services dip
Over the past three reports, indicators of friendliness and professionalism at facilities have been trending in the wrong direction.
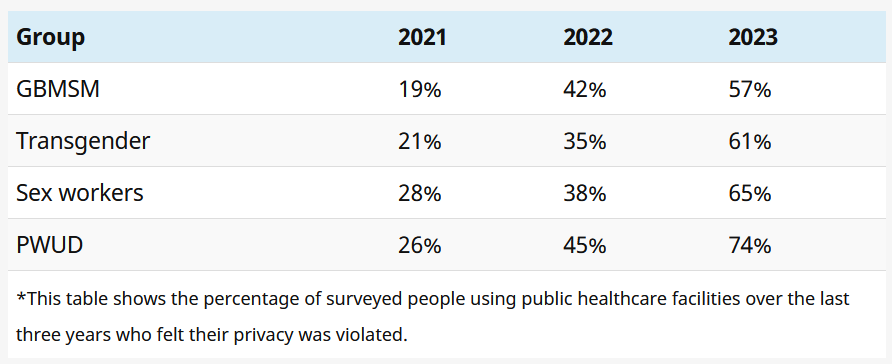
Privacy violations getting worse
Looking at Ritshidze’s figures for the past three years, there appears to be a clear trend of privacy violations getting worse. As shown in the below table, the percentage of people who did not think their privacy was well respected at the facility has been increasing year on year for all four key population groups.
Peer-led support
One way to ensure better access to public health services for key population groups is for these services to be run by people from these groups, says Jacqueline Pienaar, a psychologist and public health specialist and technical director at The Aurum Institute, an NGO.
“One of the core success factors of NGO-led facilities is that they are peer-led, which means that if it is a clinic for sex workers, it is run by sex workers, if it is a clinic for men sleeping with men, it is led by men sleeping with men. This allows the clinic to know what the health needs and sensitivities are of that particular group, which creates a more welcoming and safe space.”
Pienaar says another success factor of NGO-led clinics is that they have community advisory boards made up of key population groups who recommend how services should be provided where they are needed most.
“So it is not a top-down approach where a particular institute decides how services are going to be provided, but a collaborative, co-creation process with the community we serve where the community advisory board serves as the liaison and provides the input as to what services are needed and why people are not coming up for treatment.”
‘Understanding who you are working with’
Pienaar says some nurses at government clinics are not sensitised and don’t understand that there is diversity in sexual orientation and how people appear.
“When nurses are confronted with people who do not fit a particular social mold, they act out and they don’t understand that it is actually hurtful when you call your colleagues to come out and see a trans woman, or it is hurtful if you do not accept that the person you are seeing is a sex worker, because sex work is also a form of work,” she says.
Sensitisation at Centres of Excellence
Through the US President’s Emergency Plan for Aids Relief-funded Centers of Excellence (selected public clinics designated to provide specialised services for key populations) about 200 public clinics will be targeted in 2024 to improve access to healthcare services for key populations.
The sensitisation work involves training healthcare workers at public clinics to understand the sexual orientation spectrum of key populations. One way of ending discrimination, Pienaar says, is greater exposure of public clinic nurses to key populations through creating key population friendly-centres.
“Sometimes the nurses are not wilfully trying [to] be nasty. They have just not been exposed to working with key populations so it is foreign to them when a transgender woman walks in. They do not know what services to offer or what to ask them,” says Pienaar.

A Ritshidze clinic monitor. (Photo: Rian Horn / Ritshidze)
Ritshidze senior researcher James Oladipo believes these Centers of Excellence could be a workable solution. However, they will require additional staffing and nurses at these clinics will need to be extensively trained to deal with the complex health needs of key populations.
“Centers of Excellence have been identified among existing clinics to provide services to key populations. However, they will only be workable if they are friendly, safe and provide confidential spaces, or else key populations will not use them. These clinics will need people with the necessary expertise key populations need in order to support and instil culture change within the facility,” Oladipo says.
Access to PrEP
Ritshidze states that people in key populations are likely not to reveal their sexual orientation at a clinic because of the ill treatment they could face, and this can make it difficult to offer PrEP to them. PrEP, or pre-exposure prophylaxis, refers to antiretrovirals taken to prevent HIV infection.
Ritshidze argues that information campaigns such as putting up posters and daily talks about PrEP could help to raise more awareness.
While there has been an ongoing increase in the number of sites where staff say they prioritise offering PrEP to key populations, a less-rosy picture emerged when Ritshidze asked members of key populations whether they had been offered PrEP. Looking at the figures for the past three years in totality, the general trend is downward.
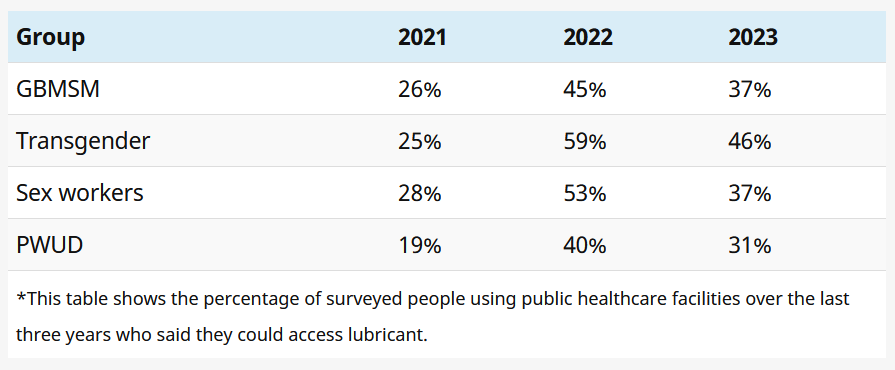
Access to lubricant
According to the report, gaps lie in many services and not only PrEP availability. While most facilities had male condoms easily available for people to take, lubricants are much harder to find. When Spotlight visited Bodibe New Clinic – a site monitored by Ritshidze in North West – the male condom dispensers were full and they had enough antiretrovirals in stock.
However, a senior staff member said she did not know where the lubricants were. The use of lubricant helps reduce the risk of HIV transmission when men have sex with men.
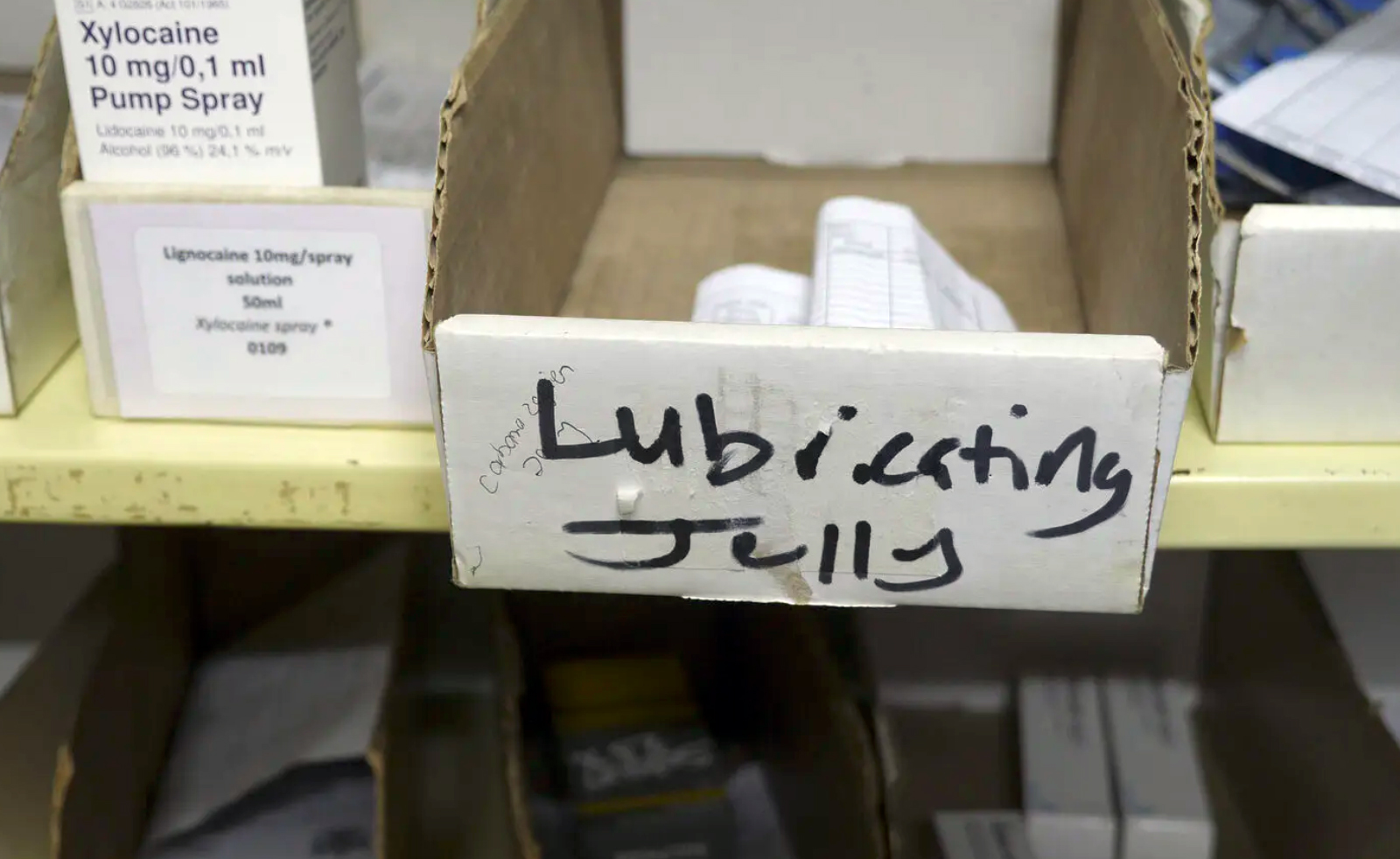
A box for lubricants at a clinic monitored by Ritshidze. (Photo: Rian Horn / Ritshidze)
She added that they offered PrEP but most of the people who tested HIV negative were not interested in taking it. She said only about one person a week was initiated on PrEP. She explained that staff didn’t receive any specialised training in how to deal with key populations, but they were trained in government ethics and had written an online test.
At facilities monitored by Ritshidze, 92% had external condoms available, only 75% had internal condoms available and just 28% had lubricant available. Lubricant availability, as measured by Ritshidze, improved dramatically from 2021 to 2022, and declined slightly in 2023.
Need for continuous training
Lynn Bust, a project manager in the Desmond Tutu Health Foundation’s LGBTQI+ and health division, says data collection and sexual orientation workshops are important to better understand the needs of key populations. She says the foundation offers a four-hour sexual orientation and gender identity (SOGI) workshop which unpacks some of the strategies to get people to start thinking about what they can do as individuals and organisations to create inclusive environments.
“Staff need to be trained on SOGI concepts and providing LGBTQIA+ affirming care. This is important not just for healthcare providers but also for support staff such as security, receptionists, cleaners and administration staff as they interact with LGBTQIA+ people and are often the first point of contact during clinics,” she says.
Bust says continuous training for people working with key populations is important. “In our experience, one training session is not enough. Rather an ongoing programme to learn about LGBTQIA+ people and their health needs is required. It takes time to change narratives, unpack stigma and dispel myths – so rather an ongoing discussion than one-off information overload.”
Bust says there is a need for explicit policies to protect not only patients but also LGBTQIA+ staff including recruitment, leave and adoption policies. “Policies should clearly prohibit discrimination based on sexual orientation, gender identity, gender expression and action to be taken against this should be clearly described.”
Bust also says data collection is important to better understand the needs of key populations. “We need national data in order to advocate for LGBTQIA+ health needs and this is severely lacking in SA. If clinics were to collect and report on SOGI, we would know more about the number of patients and their health needs to better inform the services we provide for the communities.”
The government responds
Regarding government policies, Department of Health spokesperson Foster Mohale refers to South Africa’s fifth National Strategic Plan for HIV, TB and STIs 2023-2028. Without going into detail, he says it identifies possible interventions to be implemented to address biomedical, structural and behavioural challenges faced by key populations in the country.
Mohale adds that in 2023 the department adopted a health plan to affirm its commitment to increase access for key populations to quality and friendly services. “The Key Populations Health Implementation Plan (KP-HIP): 2023-2028 promotes the establishment of KP-friendly facilities and outlines the standardised packages of healthcare services to be delivered by sensitised healthcare providers to address the needs and interests of key populations,” he says.
The department, notes Mohale, runs continuous sensitisation training sessions to empower both clinical and non-clinical employees to respect the rights of key populations and provide healthcare services in an nondiscriminatory manner. “However, it is critical to mention that change in attitudes and behaviour are long-term goals. The tangible results may take longer to be evident and realised.”
Mohale says that for the purpose of enhancing accountability facilities will continue to use complaint boxes to regularly monitor the experience of key populations. DM
This article was published by Spotlight – health journalism in the public interest. Sign up to the Spotlight newsletter.





















 Become an Insider
Become an Insider
Comments - Please login in order to comment.