SPOTLIGHT IN DEPTH
No work, full pay – why an Eastern Cape TB hospital closed and what this means for healthcare in the province

Two years ago, Orsmond TB Hospital in Nelson Mandela Bay closed its doors as a result of dwindling patient numbers. This made headlines after it emerged that 45 staff members were still being paid despite the closure. Spotlight takes a closer look at the situation at Orsmond and the wider trend of TB hospitals being closed or repurposed.
In 2021, Orsmond TB Hospital in Nelson Mandela Bay closed its doors after patient numbers dwindled. The Eastern Cape Department of Health decided to repurpose it as a psychiatric facility, but it appears little progress has been made with this transition.
Since the closure of the facility, government has spent more than R67-million on salaries for 45 former Orsmond staff members who refused to be transferred to other facilities in the same district. This emerged recently in the Eastern Cape legislature after DA MPL and spokesperson for health in the province, Jane Cowley, posed a question on the matter to Health MEC Nomakhosazana Meth.

Eastern Cape MEC for Health, Nomakhosazana Meth. (Photo: Hoseya Jubase)
“Employees were afforded an opportunity to choose the facilities they prefer to be placed at. The process was done and completed, but 45 employees refused to be allocated as per the advice given by their respective unions,” Meth said.
“A process of managing the labour dispute is underway. An agreement has been reached with workers that in the interim, whilst the bigger organisation-wide service delivery optimisation and organogram is under review, the remaining staff will be gainfully employed. All administrative matters pertaining to the situation will be applied.”
A spokesperson for Meth, Mkhululi Ndamase, confirmed that staff at Orsmond have been paid their full salaries and benefits since the closure of the facility two years ago.
“The department continues to engage with trade unions with a view of finding a solution to this impasse. The department is concerned about staff shortages and is doing its best to address it, including employing new staff and taking employees where they are most needed,” said Ndamase.
Cowley, however, said, “Until the issue of staff relocation is resolved, nothing will happen at that facility. The only thing that will follow is the hospital being vandalised and all the expensive equipment being damaged because the department is too hesitant to make a decision.
“Those individuals should have received written warnings, as the department cannot afford to pay people who are not performing any task.”
A trend of closing TB hospitals
The closure and repurposing of Orsmond TB Hospital is not an isolated incident. Earlier this year, Spotlight reported on the repurposing of three TB facilities in Mpumalanga.
Also in the Eastern Cape, Empilweni TB Hospital in New Brighton was closed in 2020 as Covid rates were skyrocketing in Nelson Mandela Bay. It has since been converted into a district hospital.
On 1 July this year, Makhanda’s only TB hospital, Temba TB Hospital, also shut its doors. The facility was housed in a building rented from the Grahamstown TB Care Society. According to the provincial government, it was too expensive to provide the service in the rented facility. The 31 staff and patients have since been moved to a wing at the busy Settler’s Hospital, in the same town.
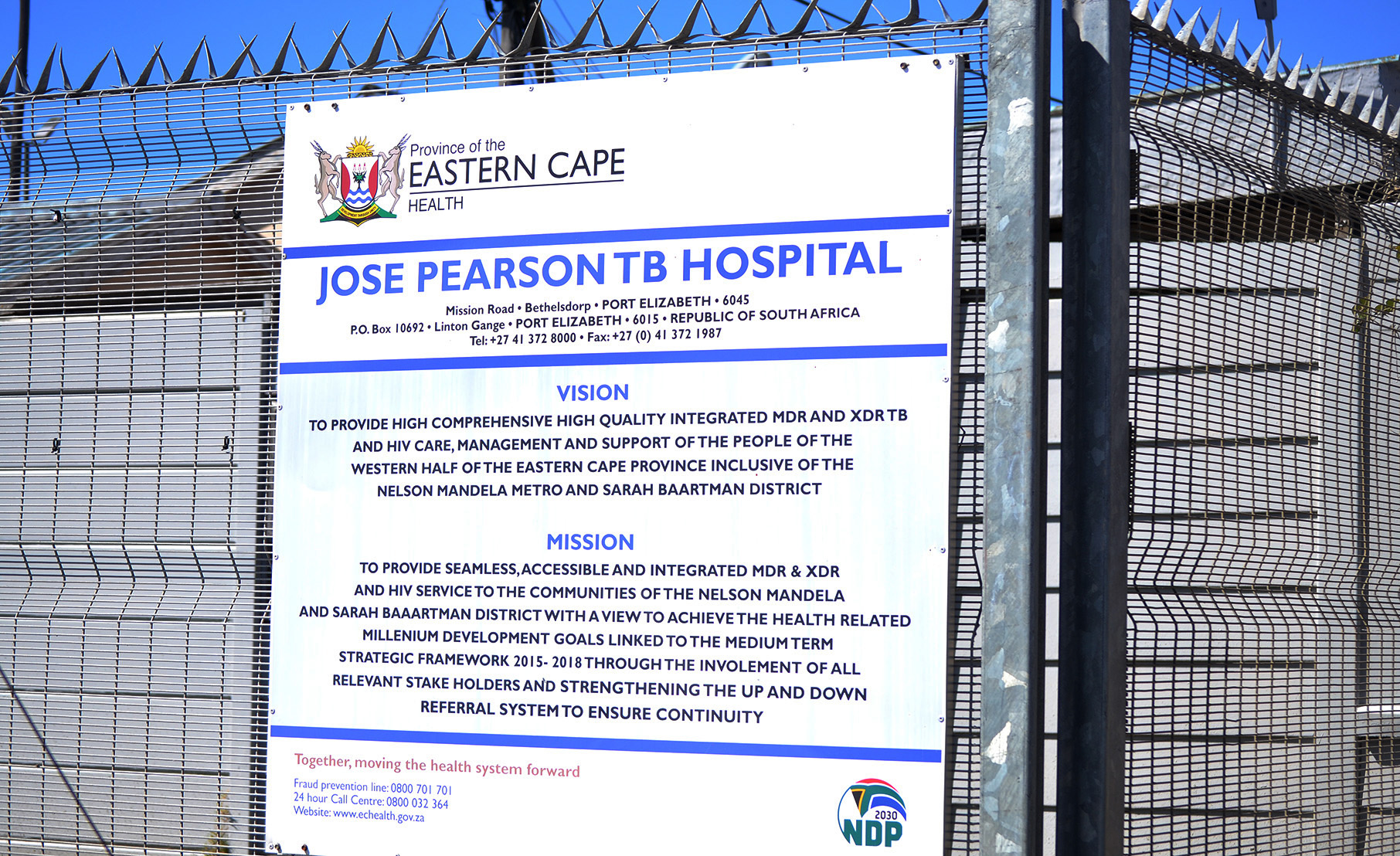
At least two TB hospitals in Nelson Mandela Bay and one in Makhanda have been closed, leaving only one dedicated TB hospital – Jose Pearson Hospital in Bethelsdorp – that also has its challenges. (Photo: Luvuyo Mehlwana / Spotlight)
The only remaining dedicated TB hospital in Nelson Mandela Bay is the 227-bed Jose Pearson Hospital in Bethelsdorp. But, as Siziwe Ntsabo, acting CEO of Jose Pearson, told MPLs during an oversight visit on 7 September, the hospital has its challenges – challenges that were exacerbated by the transfer of patients from Empilweni and Orsmond.
“Among the hospital’s problems is limited oxygen supply in the wards, broken windows and blocked plumbing,” said Ntsabo.
“Since 2019, 61 jobs have been vacant at the hospital, including executive, operational and quality assurance positions.
“Despite operating without a board, the hospital has a 72% treatment success rate. This is attributable,” said Ntsabo, “to the new (DR-TB treatment) regimen, which consists of bedaquiline, pretomanid, linezolid and levofloxacin, reducing the number of tablets patients have to take from 2,918 to 734 per treatment course.”

The Jose Pearson Tuberculosis Hospital is the only remaining dedicated TB hospital in Nelson Mandela Bay with a bed capacity of 227. (Photo: Luvuyo Mehlwana / Spotlight)
Reduced need for TB hospitals
Last year, in her budget speech on 15 March, Meth said low levels of hospital admissions for TB, coupled with a lack of district hospitals and psychiatric facilities in the region, are behind the decision to close and repurpose TB hospitals.
“In Nelson Mandela Bay, there are three TB hospitals, and yet there are only 118 patients requiring hospitalisation in the region,” Meth said at the time.
“There is no district hospital and no psychiatric facility in the region. In this region, it appears to be rational to consolidate the TB patients into one facility and repurpose the other two facilities to meet the need for a designated district hospital as well as a psychiatric facility in the district.”
One reason for the reduced demand is simply that TB rates are declining.
According to the department’s 2021/22 Annual Performance Plan, the number of new TB cases in the province dropped from 976 per 100,000 in 2014 to 747 per 100,000 population in 2018.

Eastern Cape MEC for Health, Nomakhosazana Meth said last year in her budget speech that low levels of hospital admissions for TB, coupled with a lack of district hospital and psychiatric facilities in the region, were behind the decision to close and repurpose some TB hospitals. (Photo: Luvuyo Mehlwana / Spotlight)
Meth said in last year’s budget speech that, by last year, the department reached 92/91/79 on its TB targets, meaning 92% of people with TB have been tested, 91% of those were initiated on treatment, and 79% of those were successfully treated.
“The decision to close TB hospitals has been informed by the fact that patients needing hospitalisation have, in the recent past years, been consistently going down,” said Ndamase.
“The low-bed utilisation rate is attributable to the efficacy of the therapeutic agents that we are using to treat our drug-resistant TB patients. Also, the use of the GeneXpert diagnostic test, which is a rapid test for the diagnosis of TB and Rifampicin resistance, has contributed to good progress for TB patients.
“This means individuals who have TB are diagnosed before they are sick and are started on treatment. With these developments, a lot of patients do not qualify for admission to a hospital because they are treated at a clinic closer to their homes.
“Even our state-of-the-art 120-bed Khotsong TB Hospital (in the town of Matatiele in Alfred Nzo District) has only 12 people currently being treated for TB. Same as Themba TB Hospital where bed utilisation was low at 10 patients,” said Ndamase.
The closures are also a result of a policy introduced by the National Department of Health in 2011, and updated in 2019, whereby several previously centralised TB services were to be progressively decentralised to primary healthcare facilities.
In an article co-authored by Dr Norbert Ndjeka, who leads the National Health Department’s TB programme, the authors describe decentralisation as an approach to bring TB services closer to communities with screening, testing and treatment where people live.
Decentralisation of TB services, the authors write, has “produced better treatment outcomes for DR-TB patients in South Africa and helped reduce the cost of DR-TB care”.
Shifting resources
The idea to close these hospitals makes sense if one looks at the TB cure rates, according to a former matron with 34 years of experience working in three TB hospitals in the province. She spoke to Spotlight on condition of anonymity for fear of reprisals.
“The Orsmond TB hospital also suffered from poor maintenance and was not a safe place for patients and staff. It would be beneficial if the department would channel resources from these closed hospitals to other areas that need them most, given its dire financial situation,” the former matron said.
“These resources are much needed in primary healthcare, as that is where most TB patients are tested and treated. People need to be educated in their communities that TB is a deadly disease, but with proper care, it can usually be cured, and there will be no need for patients to be hospitalised.
“Most patients can be treated at home and manage their own treatment, but if they are not taking pills, TB can be fatal. It can also morph into drug-resistant strains,” she said.
“Consultations are ongoing with social partners regarding the repurposing of facilities,” said Ndamase.

A policy introduced by the National Department of Health in 2011, and updated in 2019, provides that several previously centralised TB services were to be progressively decentralised to primary healthcare facilities. (Photo: Luvuyo Mehlwana / Spotlight)
“It is important to emphasise that this process is being done in the best interest of the millions of people who rely on the public sector for their health and care needs. The repurposing of facilities will effectively improve service delivery.
“It would be malicious for anyone to imply that the repurposing of facilities will mean TB services have come to a halt in the province. This simply means that instead of having an entire hospital dedicated to TB services when fewer and fewer people are being admitted, sections of certain facilities will be dedicated to TB patients.”
But Cowley remains fairly sceptical.
“While millions are paid to staff sitting idle at defunct TB hospitals, there is a shortage of staff and fewer people are going out to communities to check on TB patients, resulting in a shortage of data.
“During Covid, many TB patients defaulted on their treatment, and I don’t think that all those patients have been accounted for. If it is true that TB patient numbers have dropped to the point where these facilities may no longer be necessary, then it is a good thing,” she said.
“I think the department did this to cut costs because it is not financially viable to run a hospital with low bed utilisation,” said Cowley.
“But we know that this department is not always transparent about the number of TB cases. In past years, the department effectively managed TB as a chronic disease in the province. So, it is possible that patients are being better treated and are more educated about the importance of taking their medication.”
Differing transitions
Orsmond’s transition from TB hospital to psychiatric facility has been a bumpy one. Some of Orsmond’s staff, who were sitting in an open garage at the facility surrounded by overgrown grass, refused to be interviewed by Spotlight. They accused the media of not exposing the department and highlighting their plight.
By contrast, one worker at Empilweni Hospital, who is not authorised to speak to the media, said their transfer from a TB hospital to a district hospital was “handled with care”.
“The hospital is more of a step-down hospital, as we receive patients from Dora Nginza and Livingstone Hospital. We have fewer than 30 patients, and the staff far outnumber the patients. Some of the workers don’t have any work, but they come to work for the sake of coming to work,” the staff member said.
Lunga Ntshebe, chairperson of the Grahamstown TB Care Society, said the closure of the Themba TB hospital took them by surprise.
“To keep TB patient numbers low, the department stopped admitting TB patients to the facility before its relocation. This was done to create the impression that Makhanda does not need a TB hospital.” DM
This article was published by Spotlight – health journalism in the public interest.






















 Become an Insider
Become an Insider
Comments - Please login in order to comment.