SPOTLIGHT
Hospital histories – mental healthcare at Valkenberg today … and 130 years ago

Due to policy shifts and the increased availability of antipsychotic medication, mental healthcare has become decentralised, with most patients being treated in primary and district health facilities nearest to where they live. Only about 10% of mental health patients are referred to psychiatric hospitals like Valkenberg in Cape Town. As part of Spotlight’s series on hospital histories, Biénne Huisman visited Valkenberg and gained insight into how our approach to mental healthcare has changed over the years.
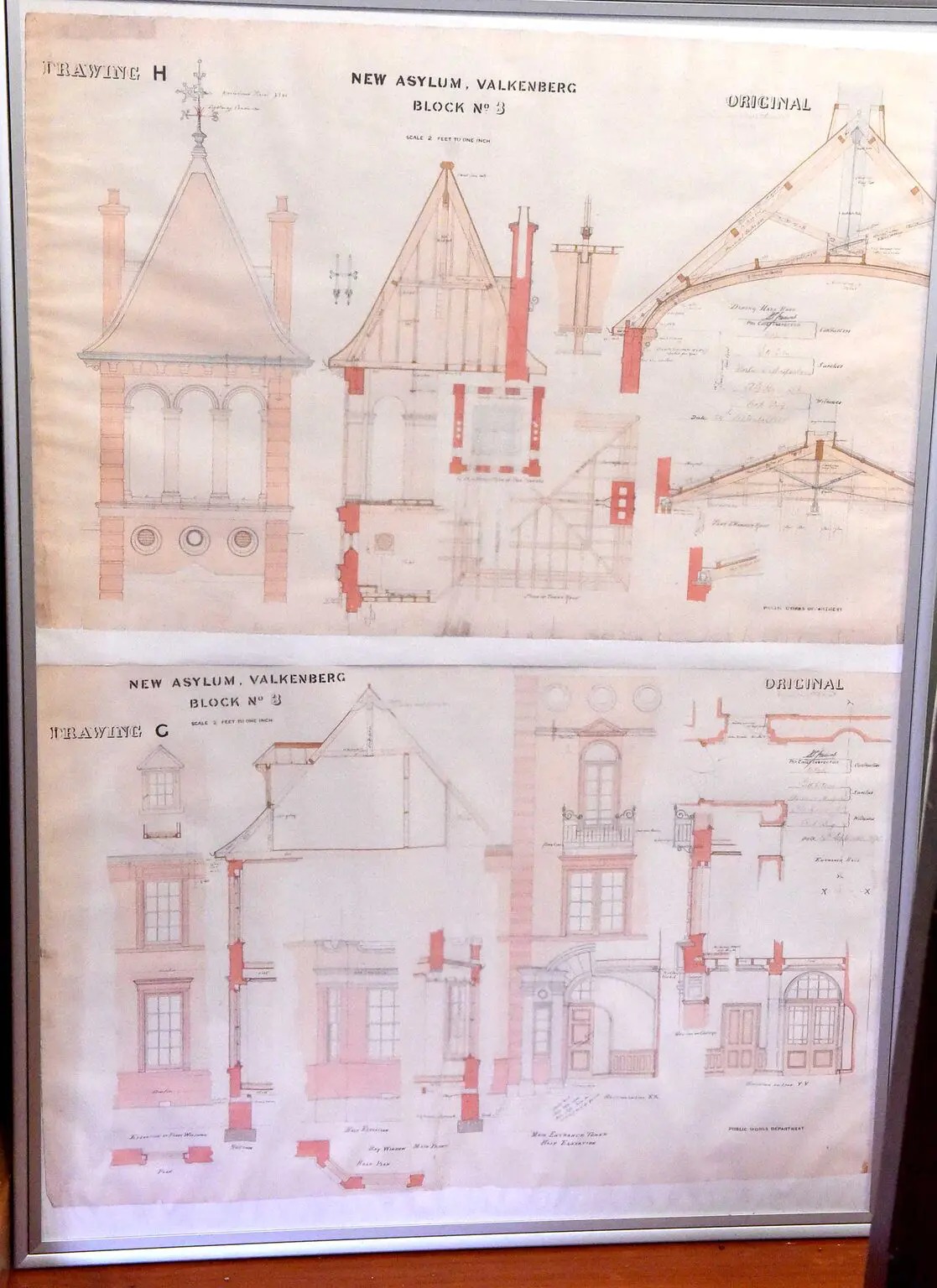
In Cape Town, between the Liesbeek and Black rivers, Valkenberg Psychiatric Hospital’s original building – dating from around 1770 – cuts an imposing silhouette. One of the area’s oldest surviving homesteads, it is three storeys high, light pink with a steeply pitched roof and one tall turret flanked by dormers. Around it, shrubs are neatly trimmed, lilies bloom in winter-wet soil and guinea fowl dash about on the lawns.
Inside the historic building, now mostly used for administration, the head of the facility’s clinical unit, Dr Qhama Cossie, and deputy nursing manager Mapitsi Photo are seated at a small boardroom table.
Photo checks their records, saying that on the day of our interview, they have 441 patients. Available beds remain a challenge at the tertiary hospital, affiliated with the University of Cape Town (UCT). Admitting referrals only, the hospital consistently runs at full capacity, with long waiting lists.
Currently, their forensic waiting list is 14 to 30 days for minor offences, and, for serious offences, 14 months. The staff include 241 nurses, 11 psychiatrists, seven psychologists, 10 social workers and eight occupational therapists.
Earlier this year, Zandile Mafe, the man accused of setting fire to the National Assembly and the Old Assembly, was sent to Valkenberg for psychiatric evaluation, where an initial mental health diagnosis was paranoid schizophrenia. He later applied to the Western Cape High Court to send him for observation at a psychiatric hospital in the Eastern Cape.
The ins and outs of admission
Explaining the admissions process for cases like Mafe’s and others, Cossie says that at Valkenberg they have two sections – clinical and forensic admissions.
“So patients enter through two different acts,” he says. “To be a forensic patient, you need to come through via the Criminal Procedure Act. So if there’s a charge and there’s a question about mental illness, that person might be sent for observation.
“Let’s say there’s a crime, but there might be mental illness involved. Then the courts rule that the accused has a 30-day observation period. Over 30 days, you are assessed by a psychiatrist. The decision that they make can be that you’re fine, that you don’t have a mental illness, or that your mental illness did not influence your behaviour. Then you can go back to court and the process can proceed.
“Or they might say that, actually, you’re not fine, you’re not well enough to appear in court. Or at the time when you committed an offence, you were sick and influenced by the mental illness. So you go back to court, but the court process doesn’t proceed. You are then made a state patient,” Cossie explains.
Then there are clinical admissions.
“We have the general side, the acute side,” he says, “where people come through under the Mental Health Care Act under which you can either be a voluntary patient, where you have an illness and you want help, and you have the capacity to make this decision. Or you can be an assisted patient where you want help, but you lack capacity. And then there’s involuntary where you lack capacity, and you don’t want help, but you are deemed to need help.”

Currently, the forensic waiting list at Valkenberg is 14 to 30 days for minor offences, and for serious offences, 14 months. (Photo: Nasief Manie / Spotlight)
Managing risk
Cossie says mental healthcare has become decentralised, with most patients being treated by general practitioners at clinics or district hospitals nearest to where they live. A contributing factor to this is the availability of antipsychotic medication. He says only about 10% of mental health patients are referred to psychiatric hospitals like Valkenberg.
“At the hospital, we manage risk,” says Cossie. “If the risk is low, then you can take treatment as an outpatient. But if the risk is high, that’s where you might need to stay at the hospital. The kind of risk varies. So there [are] people who are at risk to themselves. They might hurt themselves. There [are] people who are a risk to others, [and] there [are] people who are at risk from others, for example, someone who is vulnerable on the streets.”
The South African Mental Health Care Act was passed into law in 2004, placing the focus on human rights and the humane treatment of patients.
Cossie says the act has strict guidelines for aspects like mechanical restraint and seclusion.
“Back in the day, straitjackets and other restraining mechanisms were used. But nowadays we’ve got chemical restraints – medication. Someone who is very, very ill might need to be held down in order to give them medication. But even that is legislated. So if you do have to hold someone down, you have to report to the mental health review board. And those forms go through to a high court judge.”

In the past, straitjackets and other restraining mechanisms were used on mental healthcare patients. (Photo: Nasief Manie / Spotlight)
A glimpse inside
Around the administration building, a few other historic buildings stand abandoned, waiting to be restored. Newer buildings and wards have been added, but Cossie says infrastructure remains a challenge.
At one of the newer buildings, Photo guides us past a security guard into the clinical high-care unit where male and female patients stay in separate wards. The foyer is decorated with fabric applique art. It is quiet, with empty, gray chairs – visiting hours are only later, from 2pm to 4pm.
Visitors’ rules posted against the wall dictate that no cell phones or cameras are to be used inside and that no glass bottles or tins are allowed.
In the women’s high-care ward, 27 patients are presently being treated for various illnesses, including borderline personality disorder, schizophrenia and bipolar disorder.
At the time of our visit, the patients are seated at tables having lunch. Many are wearing dressing gowns – these are handed out because of the winter cold, a nurse explains. The seclusion room, where patients might be kept while medication takes effect, has a mattress and a heated floor. Patients at high risk to themselves are not allowed to wear clothes inside the seclusion room, the nurse explains, as they might use the garments to hurt themselves.
Past and present
In the historic administration building, Photo guides us past another security guard along a corridor with wooden floors, past an old marble fireplace and forensic observation consultation rooms, to Valkenberg’s museum inside a sunlit room.
Here, obsolete equipment and surgical tools are on display, along with old staff photographs and framed extracts from a visitors’ rule book dated 1927. “Visitors should be careful not to make any promises to patients or to excite hopes that cannot be fulfilled…” reads the document.
Adjacent to the museum room is a former isolation room – its walls and door padded. A straitjacket with leather straps is draped over a chair next to a stretcher carved from wood. Also on display is bulky equipment used for administering electric shock treatment, a source of controversy in the past following depictions such as in the 1962 Ken Kesey novel One Flew Over the Cuckoo’s Nest, later made into a film.
Photo explains that these days electroconvulsive therapy (ECT) is administered under general anaesthesia.
“It is used when patients do not respond to other treatments,” says Photo. “We do it in theatre here. Patients are put to sleep with anaesthesia and then electrodes are applied. It is effective. It works.”
ECT is available in South Africa’s private and public sectors and is used around the world for treating major depressive disorders or mania in people who do not respond to other treatments. The procedure sees small electric currents pass through the brain, intentionally triggering a brief seizure. It is believed this can cause changes in brain chemistry, reversing symptoms of some mental health conditions.
Valkenberg’s museum reflects how attitudes to mental healthcare have changed over the years.
Last October, at an event to mark Valkenberg’s 130th birthday, (postponed by a year due to Covid) government officials revisited the facility’s “scandalous” past, noting how much had changed.
At the event, Valkenberg principal specialist Prof Sean Kaliski said, “This hospital has come through many scandals. When I arrived in 1989 it had about 2,000 beds. Most of the wards had chronic patients living in abysmal conditions … It was horrendous under apartheid. Many of the staff were denigrated, humiliated.”
During apartheid, black and white patients were separated.
“The hospital used to be on two campuses,” says Cossie. “So there’s this Observatory campus, which was for white patients, and then there’s also the Pinelands campus, across the freeway – the Oude Molen side – that used to be the non-white side of the hospital.”
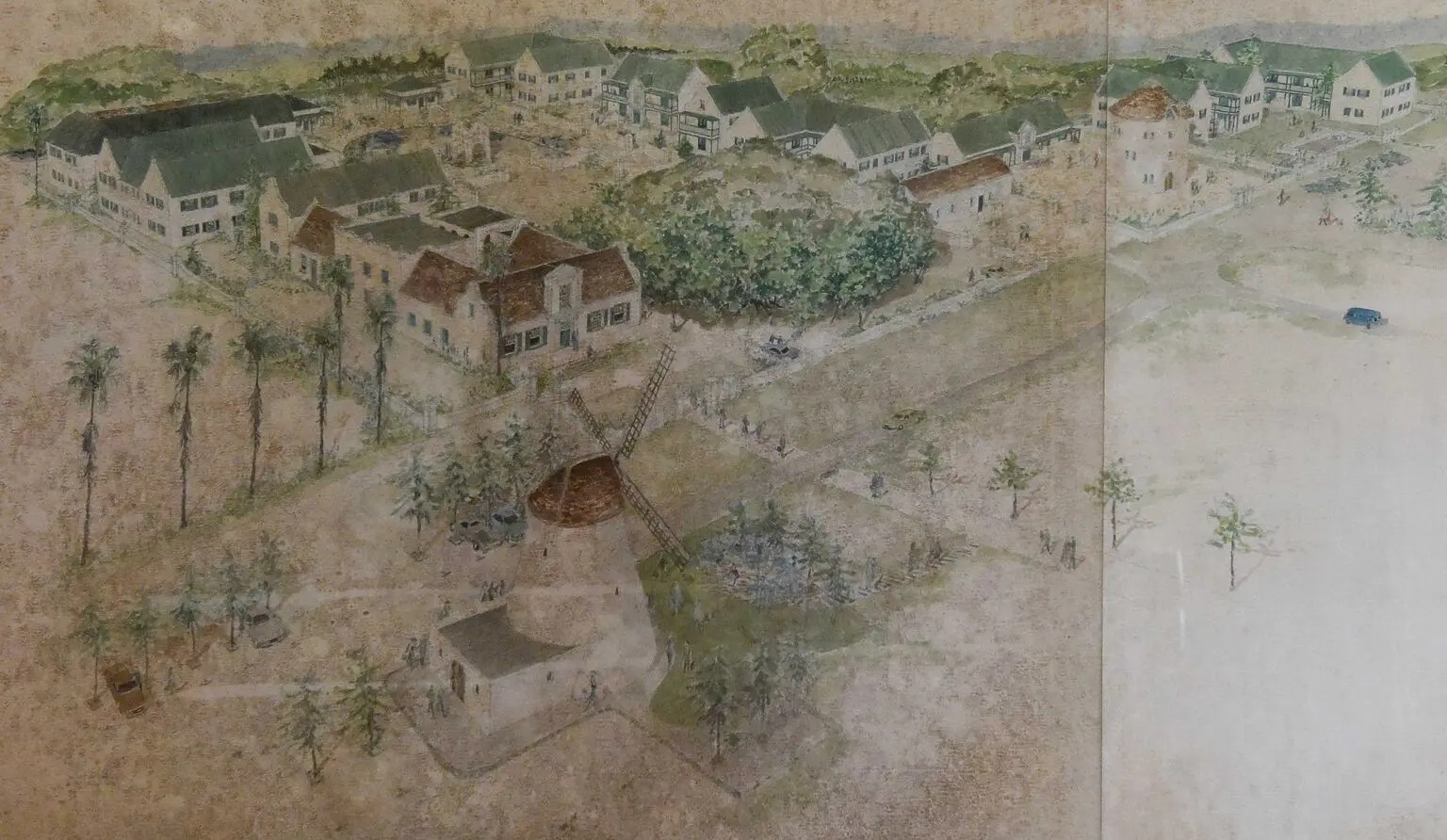
In 1891 modifications were made to the werf (farm yard) and existing buildings to accommodate the first 250 psychiatric patients housed at Valkenberg Hospital. (Photo: Valkenberg Museum)
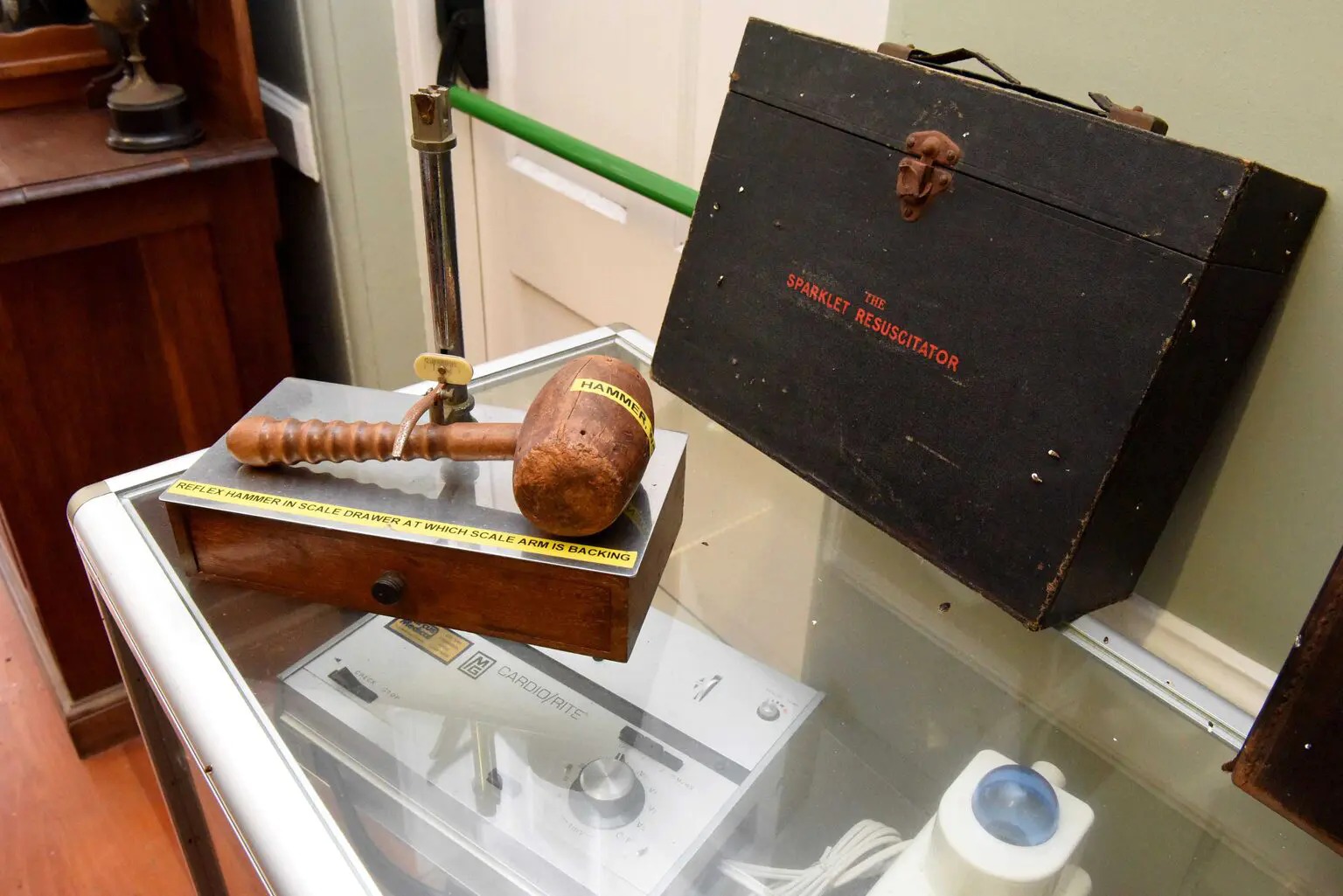
In the Valkenberg Hospital’s museum, there are old equipment and surgical tools on display, along with old staff photographs. (Photo: Nasief Manie / Spotlight)
Cornelius Valk’s estate
UCT Department of Archaeology records note that some of the earliest descriptions of the land stem from Dutch farmer Cornelius Valk’s estate in 1721, which mentions modest dwellings with “afdakjes” (a lean-to). The present building was probably built around 1770 by farmer Cornelis de Waal. In 1881, the Cape Colony Government brought the land for use as a “reformatory”.
The archaeology report, dated 1993, states: “In 1891 modifications were made to the werf [farm yard] and existing buildings to accommodate the needs of the first 250 psychiatric patients housed at Valkenberg Hospital.”
The building was declared a national monument in 1986.
Since 1994, notable improvements have been brought about by Friends of Valkenberg, a non-profit organisation founded by Francoise Robertson, wife of the then-head of psychiatric services at UCT, Professor Brian Robertson. The organisation also successfully petitioned against a Western Cape provincial cabinet proposal to close the hospital in 1998 “with the intention of rationalising services”.
Over the years, Valkenberg has had many famous patients, including anti-apartheid poet Ingrid Jonker, who was first admitted with depression in 1961. Four years later, Jonker took her own life. Jonker’s mother, Beatrice, was admitted to the institution several times too, notably while she was seven months pregnant with Ingrid, according to the poet’s biography by Petrovna Metelerkamp.
Author K Sello Duiker recalls his time at Valkenberg in his 2001 novel, The Quiet Violence of Dreams, where protagonist Tshepo is committed for cannabis-induced psychosis.
“Sometimes I just pray for the light of day when I will be able to breathe again instead of holding my breath with fear,” says Tshepo. Duiker committed suicide in 2005.
Speaking in gentle tones, Cossie says patients do get better, though. For him, what sets psychiatry apart from other medical fields is close relationships and rapport with patients.
“I think it’s more relational,” he says. “Even if someone is on medication, you need to have a relationship with them to get them to trust you to take their medication. The key ingredient is rapport.” DM
This article is the second in a Spotlight special series on the history and ongoing relevance of several old hospitals in South Africa. Not only do we find the stories of these places fascinating, we think they provide valuable cultural and historical context for healthcare services today. The first story in the series, about Brooklyn Chest Hospital, can be read here.
This article was published by Spotlight – health journalism in the public interest.






















Comments - Please login in order to comment.