SPOTLIGHT OP-ED
With the right interventions we can help many more men start and stay on HIV treatment

June is Men’s Health Month and while the focus is on men’s attitudes about their health, we have also been reflecting on the health sector’s attitudes towards men. Men are not indifferent about their health and are not inherently poor health seekers. If many of them are avoiding healthcare services, it may be because they are not getting what they need from the healthcare system.
We hear many stereotypes about men and health, but how many are true?
A few years ago representatives of the Mpilo Project spoke to more than 2,000 men in KwaZulu-Natal and Mpumalanga to understand why many find it hard to engage with HIV testing and treatment. We uncovered several myths and misperceptions.
One common myth is that men are stubborn and apathetic about HIV – that they aren’t listening and don’t care. While many men may indeed wear a mask of indifference, HIV leaves many of them feeling paralysed by fear and anxiety. This is why we need a health service delivery approach rooted in encouragement and reassurance, not scolding and pressure.
Another common misconception is that men are mainly just workers who need practical solutions like convenient clinic hours and quick service. The reality is that men are complex human beings who face social and emotional barriers as well as practical ones. We need solutions that address both practical and psychosocial barriers.
There is also a view that sources of support are available and that men just fail to access them, perhaps because “they don’t really want support”. In fact, many men are hungry for support but see no sources that feel safe or relatable. They experience counselling as scripted, one-directional, overly technical and often judgemental. The key is to give men the right sources of support and to speak empathetically to their individual issues and concerns.
We’ve also seen good progress on viral suppression… comparable to the rate among women – proof that men on treatment are fully capable of being adherent.
Finally, there is a view that healthcare providers are helping men by taking proactive approaches like provider-initiated testing and tracking-tracing. But these often leave men feeling hunted and ambushed by the health system. We need proactive approaches that leave men feeling like they still have control over their own lives and decisions and help them develop their own internal motivation to start and stay on treatment.
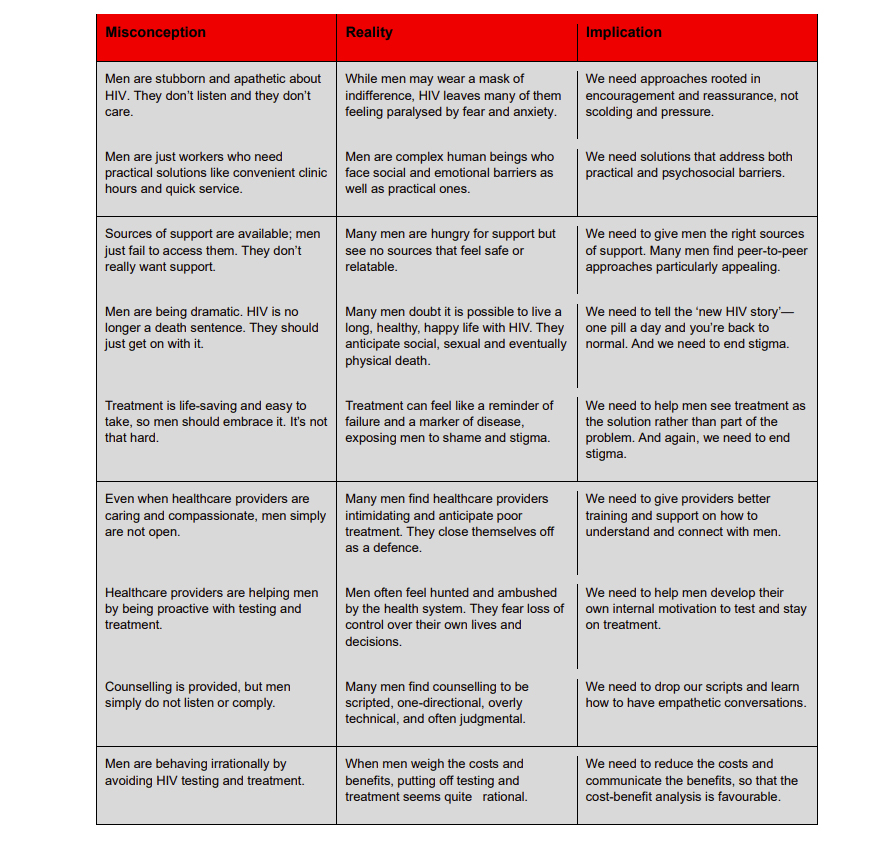
These and other misconceptions can lead healthcare providers to conclude that men are simply difficult if not impossible to reach. But once we understand their barriers, that picture changes dramatically.
The 11th SA Aids Conference concluded last week and in one of the plenary sessions we had the opportunity to respond to the question: “Strategies for reaching men – are we seeing a return on investment?”
The short answer is yes!
Since 2017, the percentage of men with HIV in South Africa who know their status has increased from 78% to 94%, nearly on par with women. We can attribute that in part to approaches like HIV self-testing that have made it quick, easy and private for men to learn their status.
Read more in Daily Maverick: HIV in graphs – latest figures confirm declining rates, but areas of concern remain
We’ve also seen good progress on viral suppression, which has increased from 82% to 93%, again comparable to the rate among women – proof that men on treatment are fully capable of being adherent.
Yet only 70% of men who know they have HIV are currently on treatment – hardly any increase at all from 68% in 2017.
Given the progress we’ve seen in men testing for HIV and achieving viral suppression, the persistent gap in men on treatment suggests that something is wrong – not with men but with the HIV treatment services and support we are offering them.

A few years ago representatives of the Mpilo Project spoke to more than 2,000 men in KwaZulu-Natal and Mpumalanga to understand why many find it hard to engage with HIV testing and treatment. (Photo: MSF / Stefan Heunis)
The good news
The good news is that we know much more than we did a few years ago about what works. Here are three examples.
The MINA campaign aims to reach men with “the new HIV story” by featuring stories from real men living a healthy, happy life with HIV on social media, television, radio, billboards, etc. The campaign also helps men feel more welcome in the clinic, using signs and materials to send the signal to men that “this is your space too”. MINA-supported districts and facilities have seen strong growth in testing and linkage, as well as modest improvement in retention in care.
We have seen that men do engage when we in the public health sector meet them where they are rather than where we want them to be.
The Coach Mpilo model employs men who are thriving with HIV as coaches of men at risk of non-initiation or disengagement. Coaches provide a safe, relatable source of support and serve as living proof that HIV is not the end of the road. Piloted in 2020 and currently implemented in 18 districts, the model is achieving 97% linkage to care and 94% retention.
The B-OK bead bottles are a simple visual tool for helping people to understand the benefits of HIV treatment and viral suppression and, more importantly, to build the motivation to start and stay on treatment. Red beads are HIV; black beads are healthy cells. A mixed bottle represents most people upon diagnosis. A red bottle represents the virus multiplying uncontrolled in the absence of treatment. A black bottle with one red bead represents viral suppression achieved through treatment adherence. In an evaluation of the tool, understanding of how HIV treatment works increased from 12.5% to 92.5%.

The B-OK bead bottles are a simple visual tool for helping people to understand the benefits of HIV treatment and viral suppression. (Photo: The Mpilo Project)

The key is to give men the right sources of support and to speak empathetically to their individual issues and concerns. (Photo: Jessica Wiggs / TB Alliance)
Men are not indifferent about their health and they are not inherently poor health seekers. If many of them are avoiding healthcare services, let’s consider that it may be because they are not getting what they need from these services.
We have seen that men do engage when we in the public health sector meet them where they are rather than where we want them to be; when we speak to their needs and priorities rather than ours; when we give them the right sources of support rather than one-size-fits-all, and when we help them build understanding and motivation rather than simply instructing.
When we invest, we see returns. Let’s keep investing in scaling what works. DM
Malone is the Project Director of the Mpilo Project, PSI.
This article was published by Spotlight – health journalism in the public interest.






















 Become an Insider
Become an Insider
Comments - Please login in order to comment.