SPOTLIGHT
Community-based testing boosts diagnosis of infectious TB, study finds
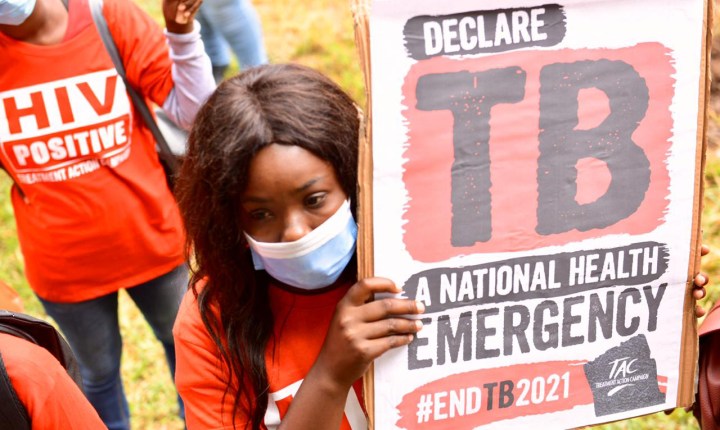
Every year, tens of thousands of people who fall ill with tuberculosis in South Africa are not diagnosed. Because of this there has been much focus on testing people earlier rather than waiting for them to show up at clinics when they are already sick. One potential solution, explored in a trial called XACT 2, is a community-based point-of-care molecular test. Tiyese Jeranji spoke to experts involved with XACT 2 and unpacks the study’s findings recently published in ‘Nature Medicine’.
Every year, according to the World Health Organization (WHO), tens of thousands of people who fall ill with tuberculosis (TB) in South Africa are not diagnosed. Globally, of the estimated 10 million people who get the disease annually, about four million never receive a positive test.
The problem of underdiagnosis was underlined by South Africa’s first TB prevalence survey, conducted mainly in 2018, with key findings made public in 2021. As Spotlight reported at the time, of the 234 people found to have TB in the survey, about 58% had abnormal X-rays without any TB symptoms, 35% had both abnormal X-rays and TB symptoms and about 7% had symptoms only.
In response, two strategies are being tried in South Africa to diagnose more people with TB more quickly. One is mobile X-ray screening – an X-ray suggestive of TB still requires a confirmatory molecular test. The other is offering people considered to be at high risk of TB an annual molecular TB test, irrespective of whether they have symptoms. In this “targeted universal testing” (TUT) approach, living with HIV, having had TB in the past year and having close contact with TB are considered important risk factors for TB. Spotlight has reported on X-ray and TUT pilot projects in South Africa.

A series of related trials called XACT are exploring community-based TB testing using battery-operated molecular tests. Testing is done using GeneXpert Edge, a portable, battery-operated version of the lab-based GeneXpert tests already in wide use in South Africa. (Photo: Nasief Manie / Spotlight)
Dr Lucy Connell, TB programme lead at health NPO Right To Care, says the mistake people often make is that they think they are not at risk of getting TB. “Anybody can get TB,” she says. “If you breathe, you can get TB.”
But the challenge with the current testing system, says Connell, is that it is passive. This means that we generally still wait for patients to arrive at health facilities once their symptoms are severe enough. Furthermore, she says, people at risk of TB and those who have any TB symptoms or a chest X-ray that suggests TB require a molecular TB test (the GeneXpert is the one used in South Africa) to confirm whether they have TB. The test requires a quality sputum sample – which some people, especially children, struggle to produce. “This is where SA is falling short,” says Connell. “There are challenges with sputum collection. Low sputum collection rates result in missing people who have TB, which undermines the potential impact of digital chest X-ray TB screening.”
The XACT model
While mobile X-ray screening is done in communities, most molecular TB tests are still done at health facilities, with sputum samples sent to labs. Now, a series of related trials called XACT are exploring community-based testing using battery-operated molecular tests, essentially taking molecular testing of sputum away from clinics and into the community. XACT stands for Xpert Active Case-finding Trial.
The XACT model comprises a mobile mini-clinic using a minivan (like a Toyota Avanza) that is run by two healthcare workers with minimal training. Testing is done using GeneXpert Edge, a portable, battery-operated version of the lab-based GeneXpert tests already in wide use in South Africa.
Spotlight previously reported on XACT 3, an ongoing trial comparing testing in the mini-clinic with sending samples off to labs.
In XACT 2, researchers compared TB testing with GeneXpert Edge with an older form of TB testing called Smear Microscopy (looking for the bug under a microscope). Sputum samples in the study were also tested using culture, which is much slower but extremely accurate and typically used as a point of reference in such studies.

Dr Shameem Jaumdally, senior research scientist at the UCT Lung Institute, demonstrates the importance of ventilation. (Photo: Nasief Manie / Spotlight)
Though molecular testing has largely replaced smear microscopy in South Africa, Professor Keertan Dheda points out that microscopy remains the frontline test in most African and many Asian countries. Dheda is a general physician, pulmonologist and critical care specialist who heads up the Division of Pulmonology at Groote Schuur Hospital and the University of Cape Town. He is also the principal investigator of XACT.
Dheda says that although both of these tests, like culture, require a sputum sample, it was nevertheless worth making this comparison. He says there is no defined diagnostic standard of care for community-based active case finding. “The aim is to detect all the infectious patients and it could easily be that smear microscopy might be as efficient as Xpert at doing this because such patients would have high-burden disease. Concurrently GeneXpert may miss a lot of low-burden disease (which is borne out by what we found because Xpert missed about 50% of the disease),” he says.
In short, he says they had to be sure that GeneXpert would comprehensively out-perform smear microscopy, especially with regard to detection of infectious patients.
The trial was conducted in Mitchells Plain and Klipfontein in Cape Town. 5,274 individuals were screened for symptoms, of which 584 with HIV infection or symptoms of TB underwent further testing – roughly half with smear microscopy and half with GeneXpert Edge. The study’s primary aim was to compare time to TB treatment initiation between the two arms. Secondary aims included assessing the feasibility of the XACT model and detection of “probably infectious” people.
Faster treatment initiation
As recently reported in the journal Nature Medicine, the researchers found that the time to treatment initiation was substantially shorter with GeneXpert Edge than with smear microscopy – a median of eight days compared with 41 days. The gap was smaller but still substantial when looking only at “probably infectious” patients – seven compared with 24 days. The researchers classified TB as “probably infectious” or not based on smear positivity, cough aerosol positivity, and the presence of cavitary disease on a chest X-ray.

The GeneXpert machines that are used to detect TB on display during a TB awareness day at Brooklyn Chest Hospital on World TB Day. (Photo: Nasief Manie / Spotlight)
These findings are promising since a major benefit of starting treatment earlier in people who are infectious is that it reduces TB transmission.
“Rapid treatment initiation remains the most effective way of rendering patients non-infectious,” says Dheda, “thus the main advantage of mobile testing is that the diagnosis of TB is made very early on in the course of disease before it is spread to other individuals.”
High and not-so-high sensitivity
One concerning finding was that only 46.5% of culture-positive study participants were on treatment 60 days after being diagnosed. “This, the researchers write, “was due to a combination of factors, including disease stigmatisation, social and health system factors that may have modulated access to treatment (for example, transport costs, impact on work), migration, and the presence of minimal symptoms that may have made individuals more likely not to initiate or continue with treatment. Indeed, we found that a higher proportion of the patients who were “probably infectious” (more symptoms and more severe disease) were on treatment compared with those who were probably non-infectious.”
The sensitivity numbers didn’t shoot the lights out either. GeneXpert Edge detected 52% of individuals with culture-positive TB and microscopy about 11%. The numbers looked more promising when looking only at “probably infectious” TB. GeneXpert Edge detected 94% of “probably infectious” patients and microscopy 23.5%.
Read more in Daily Maverick: The complex interplay between TB and liver problems
The number of at-risk people (those with TB symptoms or people living with HIV) who needed to be screened to detect one case of active TB was 18 with the GeneXpert Edge, compared with 99 through microscopy.
The GeneXpert sensitivity of 52% in XACT 2 is much lower than the 80% or higher reported in several previous trials. Dheda says this is because the microbiological burden of disease in the community where the trial was conducted is lower. “These were individuals who could have had minimal symptoms or if they had some risk factor for TB, e.g. HIV but were asymptomatic. Thus, a much larger proportion of individuals would have had a lower burden of disease below the detection limit of the assay (compared to, for example, self-declared patients who come to clinics or those who are hospitalised),” he says.

Professor Keertan Dheda, a pulmonologist and critical care specialist who heads up the Division of Pulmonology at Groote Schuur Hospital and the University of Cape Town. (Photo: Nasief Manie / Spotlight)
Dheda says it clearly suggests that more sensitive non-sputum-based tests are required for the diagnosis of TB. However, on the flip side, he points out that GeneXpert Edge detects almost all the infectious cases. He says the priority of a widespread public health intervention may not be to necessarily detect all the TB cases, but certainly to detect almost all the infectious patients who would most likely have the potential to transmit disease and hence amplify the epidemic.
Transformative potential
Professor Martie van der Walt, director of the TB Platform at the South African Medical Research Council, says the findings from XACT 2 are very promising. “It shows that when testing is brought to people in their communities, there is good uptake of services, and people with TB are started much sooner on treatment than in clinics where the result of GeneXpert is only available days later. The study showed that we should go out in communities and not expect them to come to clinics,” she says.
According to Dheda, these results are set to transform the way clinicians manage TB.

Community members at Brooklyn Chest Hospital during a TB awareness event on World TB Day this year where the team showed how the XACT model is set up. (Photo: Nasief Manie / Spotlight)

Professor Keertan Dheda on behalf of the UCT Lung Institute donated a blood gas machine to Brooklyn Chest Hospital recently. Dr Julian te Riele accepted the machine on behalf of the hospital. (Photo: Nasief Manie / Spotlight)
“Moving diagnostics right onto patients’ doorsteps to locate those in need of treatment is an enormous benefit and means patients receive direct links to care and appropriate intensive follow-up as a community-centred, transmission-interruption intervention. The technique also defines a new standard of care for Active Case Finding techniques,” he says.
But he also stresses that the XACT model is not a magic bullet and that there are many other approaches to tackling TB. “Given the huge burden of TB in South Africa and unless we change the diagnostic public health strategies, we will not impact the epidemic to any great extent. Reducing poverty and unemployment and developing an effective vaccine remains the best chance of controlling the disease.” DM
This article was published by Spotlight – health journalism in the public interest.


















Comments - Please login in order to comment.