SPOTLIGHT
What’s next after shortened TB treatment fails in key trial?
Two studies in recent years have shown that TB can be cured in four months, sometimes two, but price and other complications make these treatments tricky to implement. At a conference in Seattle last week, a major trial of an alternative four-month treatment reported disappointing findings. Elri Voigt unpacks the latest findings and asks what the prospects are now for shortening TB treatment.
The current treatment for drug-susceptible tuberculosis (TB) used in South Africa involves a combination of four antibiotics, lasts for six months, effectively cures TB and is dirt cheap. Some people, however, find it hard to complete the full six months of treatment – in some cases due to side-effects and in others because people can feel well again long before the six months are over.
Several clinical trials in the past decade or two have evaluated the safety and efficacy of shorter regimens, mostly with disappointing results. That changed in 2021 when a study widely referred to as “Study 31” found a four-month regimen to be non-inferior to the current six-month regimen. The snag, however, is that this regimen is much more expensive, largely due to the inclusion of the drug rifapentine. This rifapentine-based regimen is recommended by the US Centers for Disease Control and Prevention, and conditionally recommended by the World Health Organization (WHO), for the treatment of TB in people aged 12 and older, but is not used in South Africa’s public sector. As Spotlight reported in 2022, a four-month regimen specifically for children is set to be rolled out in the country.
One of the next big treatment-shortening studies to watch after Study 31 was called SimpliciTB, the ambitious vision of which was not only to produce a shortened regimen for the treatment of drug-sensitive TB but a single regimen that could also be used for drug-resistant forms of TB (DR-TB). But whereas the regimen may have promise for DR-TB, findings presented last week at the Conference on Retroviruses and Opportunistic Infections in Seattle, dealt a serious blow to prospects of using it to treat drug-susceptible TB.
Disappointing findings
SimpliciTB compared a four-month treatment course consisting of the drugs bedaquiline, pretomanid, moxifloxacin and pyrazinamide (BPaMZ) with the six-month standard of care for the treatment of drug-susceptible TB. While it was a randomised, controlled trial, it was also open-label, which means patients and healthcare workers knew who was on which study arm. There was also a third study arm in which the BPaMZ regimen was given to people with DR-TB, but the study did not have a DR-TB control arm. A total of 303 people enrolled in the two DS-TB arms.

Tuberculosis medication. (Photo: Nasief Manie / Spotlight)
The researchers measured two key outcomes – culture conversion (two consecutive TB culture tests being negative) after eight weeks and unfavourable outcomes (treatment failure or relapse) after 52 weeks.
Read in Daily Maverick: “TB treatment can be cut to two months for some, landmark study finds”
BPaMZ did well on one measure but fell short on the other. By week eight, 84% of those in the BPaMZ arm had negative cultures, compared with only 47% of those on the six-month arm. After 52 weeks, however, 17% of those in the BPaMZ arm had unfavourable outcomes compared with only 7% of those in the six-month arm. On the first measure, BPaMZ was found to be superior to the six-month regimen, while on the second measure, it failed to meet the threshold for non-inferiority.
According to Dr Muge Cevik, who presented the study results at the conference, there were a lot of early withdrawals in the trial – 14 in the BPaMZ arm compared with only one in the six-month arm. The picture is thus one of the BPaMZ regimen being highly effective but patients struggling to cope with the side-effects, most of which were liver-related.
“I think the way that they presented it is they were saying if you’re just looking at efficacy, this regimen is good at killing TB and curing TB,” said Lindsay McKenna of the Treatment Action Group (a New York-based advocacy organisation). “However, if you look at the regimen on the whole that’s only true if someone can tolerate the regimen, and so it’s effective but it’s not safe and therefore it’s not a good regimen.”
Dr Vidya Mave, the co-director of the Center for Infectious Diseases in Pune, India, was slightly more upbeat. She told Spotlight that BPaMZ did exactly what it was supposed to – kill TB. But she also expressed concern over the high number of toxicity events. She suggested that using pyrazinamide for four rather than the usual two months may have played a role, although more detailed study findings would be needed to see if this was indeed the case (the findings haven’t yet been published in a medical journal). Her comments are in step with a wider sense that, even though the BPaMZ regimen is too toxic to be a viable option for the treatment of drug-susceptible TB, much can be learnt from the study and a somewhat similar regimen may still have a future.
A novel approach
While Study 31, SimpliciTB and several earlier studies largely focused on testing experimental shortened regimens, a study called TRUNCATE-TB presents a novel treatment strategy rather than just a new antibiotic regimen. In short, the strategy is to treat people for a shorter period (eight weeks) and then stop treatment if people test negative and extend treatment if they do not. Treatment can simply be restarted if someone’s TB returns after they’ve stopped the treatment.

Spotlight first reported on findings from TRUNCATE-TB in November 2022 when initial findings were presented at the Union World Conference on Lung Health. Additional findings were presented last week at the Seattle conference and study findings were simultaneously published in the New England Journal of Medicine. According to this article, a regimen based on the antibiotics bedaquiline and linezolid given for eight weeks (with extension and retreatment as required) was non-inferior to the six-month standard of care. The mean treatment duration with the bedaquiline/linezolid regimen was 85 days, compared with 180 in the six-month regimen.
Read in Daily Maverick: “Why Mpumalanga is repurposing some TB hospitals and how it will streamline service for patients”
At the conference, TRUNCATE-TB lead investigator Dr Nicholas Paton presented additional data on the potential use of biomarkers to identify the patients most likely to relapse after the eight-week treatment. Paton said the rate of relapse on the bedaquiline/linezolid regimen was about 14%. People whose TB relapsed were simply put back on treatment in line with the TRUNCATE-TB strategy. “What the trial has told us is that even with that 14% relapse rate, you can manage that within this strategy and people are fine at the end.”
Visit Daily Maverick’s home page for more news, analysis and investigations
Good news is that there does indeed appear to be a biomarker that predicts whether someone’s TB will relapse after eight weeks of treatment. “We can pick people with a high disease burden on GeneXpert (a molecular TB test already widely used in South Africa) before they start treatment [and] who don’t have a high chance of achieving cure with our eight-week treatment,” Paton said. “Essentially, that could then feed back into that strategy which we published as a sort of prototype, if you like. We can now look at ways of improving the decision-making about when to stop treatment and also look at ways of improving the post-treatment monitoring so that we can simplify that and make it more accurate at picking up people who need re-treatment.”
What comes next?
Encouraging as the TRUNCATE-TB findings may be, the only alternative to the six-month drug-susceptible standard of care that is currently recommended by the WHO and the Centers for Disease Control and Prevention is the rifapentine-based regimen from Study 31. But uptake of this regimen has been slow. According to McKenna, reasons for this include supply constraints, cost and procurement challenges.
“There are these environmental issues around how currently drug-sensitive TB drugs are procured and purchased that we haven’t had to address because you haven’t had anything new [in several years],” she says. “Now we do and it’s a problem that has to be solved before we can probably have equitable access to the four-month regimen.”
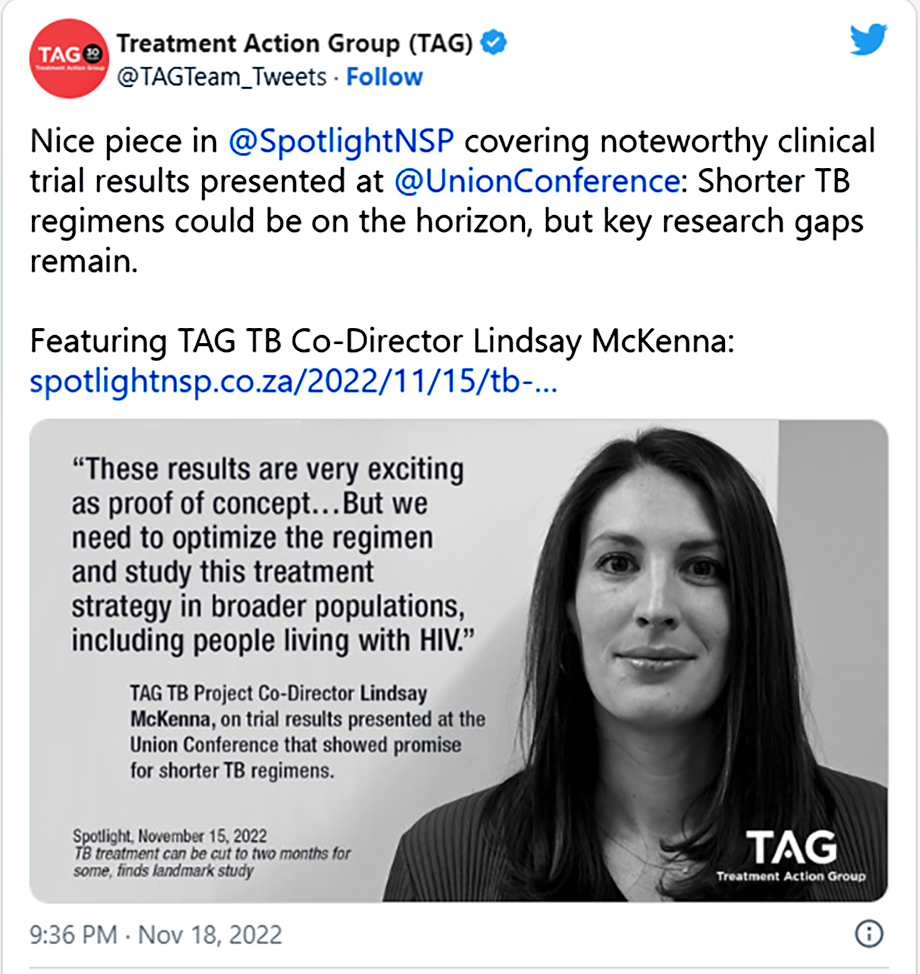
As for future treatments, McKenna suggested it is possible that research has reached the limits of how short treatment for DS-TB can get with the existing crop of new and repurposed drugs. The next wave of drugs, including advantaged alternatives to existing TB drugs, might help shorten treatment duration, she said.
Read in Daily Maverick: “As with Covid-19, the effects of TB can linger long after it is cured”
The Center for Infectious Diseases’ Mave said there are a large number of chemical entities with the potential for treating DS-TB, between 26 and 30, and it is now the job of researchers to find out what combination of these drugs would have the least toxicity, be more efficacious and easy to roll out in programme settings.
“I’m hoping within this decade we will know how low [in treatment days] we can go for DS-TB treatment,” she said.
McKenna also pointed out that the WHO is trying to address how to balance the interplay between the cost and safety of future shortened DS-TB regimens. “WHO is doing a process right now to put together an update to their target regimen profile. It’s out for public comment. It tries to weigh some of these questions. The indicators are price, safety [and] duration. They try to come up with what are the ideal minimal, optimal scenarios to help guide developers,” she explained. “What I feel is missing from some of these processes that help set the vision for what we want and that direct development and investment, is rigorous work to understand patient preferences. People with lived experience who have taken these drugs, who will take these drugs – what are their priorities and how would they rank different parts of that target regimen profile? That’s what’s missing.” DM/MC
This article was published by Spotlight – health journalism in the public interest.
















Comments - Please login in order to comment.