OP-ED
Better data is first step in improving services for persons with disabilities

South Africa ratified the UN Convention on the Rights of People with Disabilities in 2007 — but the data needed to track the implementation of the convention in South Africa is often incomparable across sectors, of low quality, or completely lacking. This limits civil society’s ability to hold the government accountable and makes it impossible to ensure equity for marginalised groups in how government plans, budgets, and implements services, argues Rural Rehab South Africa’s outgoing chair, Maryke Bezuidenhout.
South Africa remains one of the most unequal societies in the world, with inequalities, including in health access and outcomes, drawn along racial, geographical, and socioeconomic lines.
People with disabilities remain some of the most vulnerable and marginalised in society. Recent household and census data indicate that they remain poorer, with less access to government services, including health, social services, and education, than their non-disabled counterparts. A review of disability and rehabilitation data in the 2020 South African Health Review showed gross discrepancies in access to assistive devices across provinces, with unacceptably low coverage rates overall.
South Africa ratified the UN Convention on the Rights of People with Disabilities in 2007, requiring routine reporting on progress made — an exercise made extremely challenging by the lack of comparable disability data across sectors and the low quality of data within each sector, including the health sector.
A relatively new initiative by the Department of Social Development (DSD), StatsSA, and the World Bank attempted to engage government departments around the need for the harmonisation of disability determination and data collection to improve monitoring and build accountability around service delivery for this vulnerable group. This initiative is now driven by the Department for Women, Youth, and Persons with Disabilities.

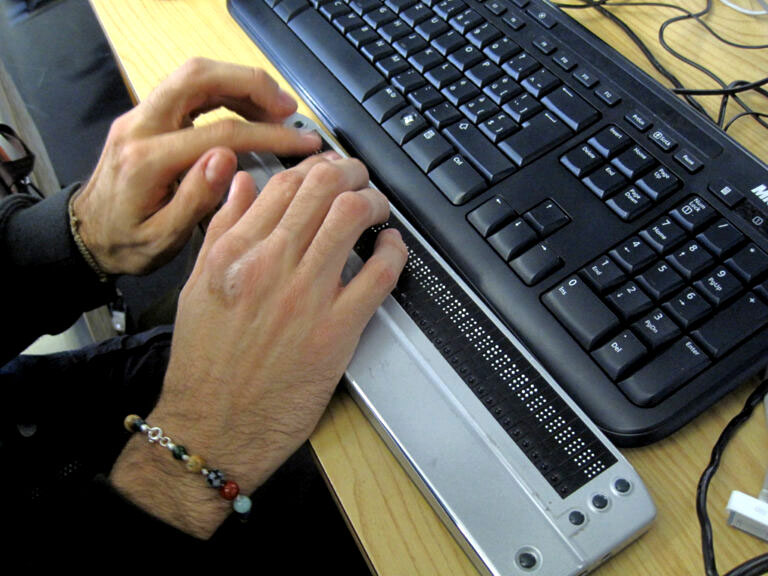
South Africa ratified the UN Convention on the Rights of People with Disabilities in 2007, requiring routine reporting on progress made but this is made difficult by the lack of comparable disability data across sectors and the low quality of data within each sector, including the health sector. (Photo: Bruno Sanchez-Andrade Nuño / Flickr / Spotlight)
This disability data harmonisation effort should be supported by disability researchers familiar with disability data collection, by other government departments and further capacity-building and funding is needed by StatsSA for both collection and analysis of disability data. Efforts at improving accountability as well as the use of data — including the ability to disaggregate and stratify disability via type, degree of disability, geography etcetera to inform local level policy, planning, and monitoring is also urgently needed.
However, the response from other government departments has been lacklustre so far.
This lack of data limits civil society’s ability to hold the government accountable and makes it impossible to apply vertical equity for marginalised groups when planning, budgeting for, implementing, or monitoring government services. Vertical equity applies when policymakers recognise that there is an inherent inequality in (health) access or outcomes for particular sub-groups and that particular sub-groups will require additional resources or efforts to ensure that they eventually get to the same health outcomes as the general society. But, without disability-related questions in key service surveillance, there is no data and information on disability to inform sectors to assess equity and monitor the inclusion of vulnerable sub-groups. These sub-groups are then simply ‘invisible’ in the data and lost among the many pressing issues of the general population.
From bad to worse
South Africa embarked on a sudden and hard lockdown in response to Covid-19 in 2020. With it, seemingly essential service providers such as the South African Social Security Agency (Sassa) and Home Affairs reduced staff numbers and services, immediately impacting the most vulnerable — particularly those without the relevant paperwork or those with applications currently ‘in process’. Even with food parcels eventually being distributed during lockdown, it was evident how little community mapping had been done on a routine basis prior to the pandemic. With the health department, however, there was no nationally communicated contingency plan regarding service delivery for people with disabilities.
Despite people with disabilities participating in the government’s Covid-19 crisis committee and the Presidential Working Group on Disability providing recommendations, key policy documents failed to directly speak to disability. One of these guiding policy documents — the Allocation of Scarce Resources during the Covid-19 Public Health Emergency in South Africa — used an assessment scale that automatically and erroneously classified people with moderate and severe mobility and cognitive impairments as having a poor prognostic outcome. Although challenged and amended, the lack of broader stakeholder inclusion when drafting policies and guidelines can lead to incorrectly restricting access to care and resources for vulnerable groups.
Siloed and left out
The organisational culture within the Department of Health, along with a historically siloed approach to service planning and delivery, and an often narrow approach to healthcare delivery focusing on preventative and curative care offered by a limited number of health professionals consistently fails to recognise or include disability and rehabilitation in essential health policy and planning initiatives.
With the medical model approach, disability is regarded as a physical problem that could be fixed or that requires a health intervention to ameliorate it. A social model of disability, on the other hand, recognises that the problem lies within a disabling society and requires a human rights-based intersectoral approach to addressing the barriers faced by people with disabilities (and the subsequent inequality they experience). This fits in with the current understanding that the social determinants of health impact health outcomes far more than medical interventions. The social determinants of health are intersectoral and political. They are the structural inequalities in our society — just as the barriers determining equality in health and socioeconomic outcomes for people with disabilities are structural in nature.
Intersectional collaboration is not South Africa’s strong point and the way in which budgets are allocated and government departments are structured does not help.

People with disabilities remain some of the most vulnerable and marginalised in society. (Photo: Black Star / Spotlight)
Ill-equipped and fragmented
As mentioned previously, there was no nationally communicated contingency plan by the national health department to ensure service delivery was sustained for people with disabilities during different levels of lockdown. With many provinces also silent on this issue, therapists and managers on the ground were left to make their own decisions which led to varied approaches that were often heavily influenced by hospital management.
Decades of underinvestment in disability and rehabilitation services and a lack of recognised staffing post establishments meant that services prior to the pandemic were already highly fragmented, poorly organised, largely centralised to hospitals (and, at best, clinics), and of variable quality. Few departments have a full multi-disciplinary rehabilitation team, few provide outreach services beyond clinic visits, and few have sufficient or appropriate databases or systems in place to actively monitor service delivery and programme performance for high-risk groups.
Visit Daily Maverick’s home page for more news, analysis and investigations
From discussions on a number of platforms and also informally with colleagues, the response to lockdown by rehabilitation departments was highly variable — some shut shop, some reduced staffing or introduced shifts, and many restricted services to inpatient treatments only.
Few departments — even if they had wanted to — had the staff, vehicles, or systems to identify and prioritise households at risk, monitor the provision of consumables and medication required by many clients with disabilities, or rapidly decentralise services to household level. Supply chains for assistive devices were and still are completely disrupted, and together with the cancellation of outreach services, already poor service and assistive device coverage rates went from bad to worse.
Caught napping
When the pandemic hit, South Africa’s public sector was caught napping with broken and incompatible systems, little community footprint, and a backlog in service delivery that should have been addressed systematically in the last 30 years. Decisions around a hard lockdown failed to appreciate the lack of preparedness by government services on the ground to roll out relief measures for the poorest. It turned a blind eye to the complete lack of intersectoral collaboration. Unable to address the social determinants of health during a pandemic, it threw the army at the problem instead.
Whilst we still have no real-time data on rehabilitation staffing levels, one positive response to the pandemic was the contracting of Covid-relief therapists who were placed in institutions at all levels of the system. Where used judiciously, they allowed permanent therapists to concentrate on building better systems and expanding outreach services. Institutions should be given the funding to absorb them now.
Recent household and census data indicate that people with disabilities remain poorer, with less access to government services, including health, social services, and education, than their non-disabled counterparts. (Photo:: Visual Pun.ch / Flickr / Spotlight)
Urgent attention is also required in rehabilitation human resource mapping. This means putting in place rehab staffing organograms based on population need (not utilisation rates) at all levels of care and rurality. Filling these posts must respond to the need for sufficient, appropriate, and appropriately skilled rehabilitation staff at primary healthcare level, as well as employing end-users in service delivery itself, such as peer supporters and parent facilitators. These peer supporters and champion mothers of children with particular disabilities, including cerebral palsy and autism, for example, can be trained and integrated into health or social services. These end-users are invaluable in establishing communication and support networks as well as improving quality of care by ensuring that interventions are contextually appropriate and that care is coordinated.
Where there has previously been little or no attempt at inclusive engagement in guiding emergency responses, we welcome the inclusion of people with disabilities on the national crisis committee. We hope that not only recommendations of mainstreaming disability across all sectors and programmes and increasing end-user engagement are taken and implemented, but that the voices of people with disabilities from rural and underserved areas are heard, and not just the privileged few. To achieve this, the knowledge and attitudes of decision-makers and those in charge of budgets toward disability must change.
The organisational culture and channels of communication within government departments must also change and a sustained approach towards building capacity and inclusivity within municipal forums and health boards and committees must happen.
Improve data
Finally, in South Africa, we too often try to make the person fit the service rather than designing the service around the person. This approach largely ignores the multiple barriers vulnerable groups face in accessing and remaining in care and deflects attention from the need for intersectoral collaboration in addressing the problems at hand.

Despite people with disabilities participating in the government’s Covid-19 crisis committee and the Presidential Working Group on Disability providing recommendations, key policy documents failed to directly speak to disability. (Photo: Victor Phung / Flickr / Spotlight)
We cannot ignore the impact that our current systems and services have on driving and perpetuating inequalities. For example, in the current system, services are centralised, so the cost falls on the patient to get to these services and this disproportionally affects people with disabilities. Where there is poor coordination of care, patients are often subjected to numerous appointments with different health professionals on different days, exponentially increasing transport costs, which is, again, worse for people with disabilities. Also, this poor coordination of care can lead to duplication of effort, and promises of home visits or assistive devices may not be acted on because of poor handover or lack of accountability by health professionals. All of these mean that the system itself worsens the quality of care and access to care as well as driving poverty among the most vulnerable.
Current health systems are largely passive, relying on the patient to initiate contact with the system. Data is often inadequate to derive a denominator or monitor coverage rates for particularly vulnerable populations — and we can only pray that health system reforms and processes underway in preparation for NHI are able to address this. Covid-19 has shown us the sheer scale of the unmet need in communities, yet it is all too easy to simply slip back into practices that drive and perpetuate inequality as health utilisation rates return to pre-Covid levels and budgets and resources are further reduced.
And without data and information, no one will be the wiser. DM/MC
*Bezuidenhout is the outgoing chair of Rural Rehab South Africa (RURESA) and a qualified physiotherapist. This article is based on her address at the recent 2022 Rural Health Conference in Oudtshoorn.
*This article was published by Spotlight – health journalism in the public interest.



















Comments - Please login in order to comment.