SPOTLIGHT
Women in Health: ‘I don’t like seeing anybody treated unfairly,’ says new head of HIV Clinicians Society

Juliet Houghton was recently appointed CEO of the Southern African HIV Clinicians Society. As part of Spotlight’s Women in Health series, Bienne Huisman spoke to her about her life working in HIV, her new role at the clinicians society, the importance of being able to laugh, and the Shakespearean origins of her name.
Describing her new job as CEO of the Southern African HIV Clinicians Society, Juliet Houghton quotes the late Archbishop Emeritus Desmond Tutu: “There is only one way to eat an elephant – one bite at a time.”
Over Zoom from Durban, Houghton is finishing her breakfast – scrambled eggs on toast – as we start the interview.
“Look, I’m very pragmatic,” she says. “Of course, there are problems and barriers, but we have to move forward. It’s about having a solutions focus to systems and breaks in systems – which of course is what we’re confronting in South Africa’s public health space. The chunk-by-chunk of the elephant applies because it can be overwhelming if you look at the big picture.”
From Warwick to Romania to the beaches of Durban
After 15 years of being based in South Africa, Houghton, born in Warwick, UK, appears comfortable drawing on African wisdom.
Qualified as an HIV nurse specialist at London’s School of Hygiene and Tropical Medicine in 1999, and as a social anthropologist at Brunel University London in 2005, Houghton’s clinical and non-profit HIV experience stretches from the UK to Romania and finally to South Africa. She featured in the 2007 documentary HIV & Me, in which Stephen Fry, a British actor, writer and broadcaster, reflects on HIV in the UK and sub-Saharan Africa.
From 1998 to 2007, Houghton treated babies and children living with HIV at Leicester Royal Infirmary in the English county of Leicestershire.

The injectable antiretroviral, cabotegravir (CAB-LA), is aimed at protecting those most at risk of HIV infection. (Photo: iStock)
“I first got involved in HIV back in the late 1980s when I was a student nurse. Leicestershire Aids Support Services had just started up, so I trained to be a volunteer with them. Most of my career was in Leicester, a city actually very much like Durban, very multicultural. Leicester has a very large Indian sub-population, and a lot of African people too – Zimbabwean asylum seekers and a Somali community, people fleeing civil war. So, coming to Durban felt very much like being at home, but with sunshine and a beach…
“I did my master’s in social anthropology of childhood because I had all these different communities that I was working with. And I thought it would really help to be able to unpack the cultural elements of their health and how they understand the United Kingdom and how to help them best fit in,” she says.
Houghton visited Romania in the early Nineties. “In Romania, children were put in orphanages for a variety of reasons. Sometimes parents couldn’t afford to keep them. Some were put in orphanages because parents feared that they might have HIV – so, because of the stigma. But alarmingly, often medical practices within the orphanages exposed the children to the risk of HIV. So again, it was a lot around educating the orphanage staff on caring for children, for example, how to take blood properly. As we didn’t have ARVs then, it was much more of a palliative care approach, managing pain and so forth. And then, fortunately, when ARVs came along, it transformed the children’s outcomes.”
What motivated her career choices?
“I don’t like seeing anybody treated unfairly,” says Houghton. “And when HIV came along, people were treated so poorly. I felt something had to be done to correct that. From a human rights perspective, that’s what’s always motivated me.”
34 ‘godchildren’
In a 2007 interview with journalist Carol Davis for the British journal Nursing Standard, Houghton describes her demanding job caring for children living with HIV as “simply wonderful”. She told Davis: “I love it. Treatments have changed enormously and some of my children are transferring to adult services now. It is a much happier state of play than 10 years ago. Usually, I bring good news to families, not bad.”
 To this day, she is in touch with 34 “godchildren” who are now adults living with HIV, thanks to life-saving antiretrovirals.
To this day, she is in touch with 34 “godchildren” who are now adults living with HIV, thanks to life-saving antiretrovirals.
Houghton started stints volunteering at rural KwaZulu-Natal hospitals from 2004. Three years later, what was supposed to be a six-month sabbatical in Durban culminated in permanent residency in South Africa. Today she describes the country as home.
Now, at the helm of the Southern African HIV Clinicians Society, Houghton is steering about 10,000 members – doctors, nurses, pharmacists, academics and policymakers – in promoting HIV care and sexual health advocacy in southern Africa.
Game-changers in HIV
Speaking to Spotlight, Houghton points out two recent developments in HIV prevention.
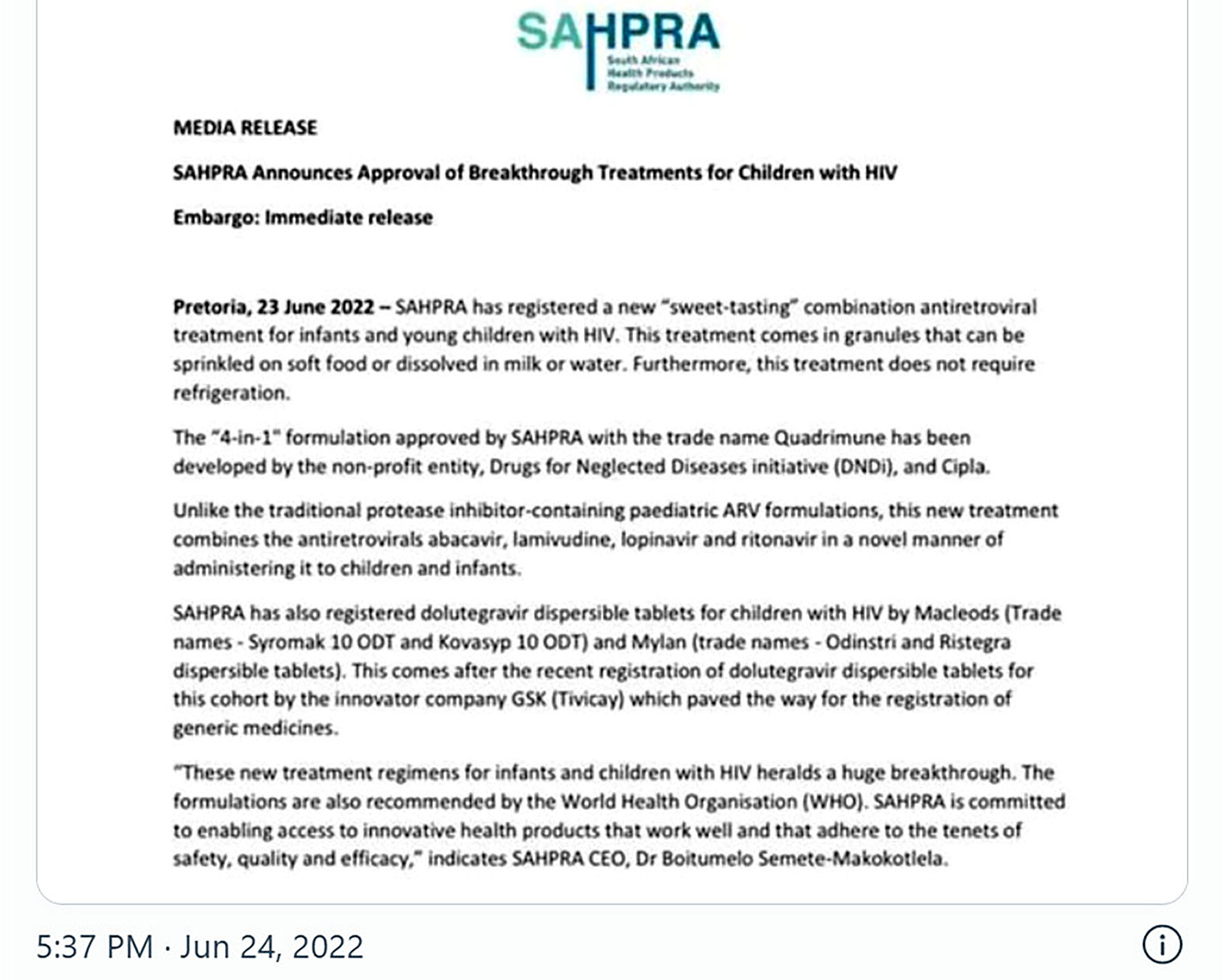
“So, we’ve already got daily oral PrEP [pre-exposure prophylaxis], which is available to everybody,” she says. “But new on the block and very exciting for women is the dapivirine vaginal ring, which women can insert themselves and which provides a month of protection from HIV infection. So that will be a real game-changer – because relying on condom use, negotiating with your partner, ultimately that can be tricky. And while we wouldn’t advocate for not using condoms, this will be just another level of protection for women.”
In March, the South African Health Products Regulatory Authority approved the dapivirine ring for use by women aged 18 and older. However, Department of Health spokesperson Foster Mohale cautioned at the time that the roll-out of the ring would be delayed while the department further assessed the effectiveness of the device.
 “And then another game-changer – injectable PrEP, the cabotegravir injection is also coming,” says Houghton. “These offer two months of protection against HIV. I think this is before [the regulatory authority] now and there are also negotiations around the costs.”
“And then another game-changer – injectable PrEP, the cabotegravir injection is also coming,” says Houghton. “These offer two months of protection against HIV. I think this is before [the regulatory authority] now and there are also negotiations around the costs.”
Spotlight previously reported on what needs to happen before this injection will become available in the public sector in South Africa.
She notes the recent announcement of an agreement between the Medicines Patent Pool (MPP) and pharmaceutical company ViiV Healthcare, allowing for generic production of the injection in 90 countries, including South Africa. The MPP has told Spotlight that it expects generic versions to hit the market in three to five years.
Parallels in stigma: Covid and HIV
In a nod to Women’s Month, Houghton adds that 64% of clinicians society members are female and about 30% are nurses.
She points out the stress placed on nurses during the Covid-19 pandemic, particularly at rural facilities.
“I think the mental health burden on our rural health workers, primarily women, has been huge. It was such a stressful time, seeing patients die because of a lack of access to oxygen, or access to an ambulance. Staff are struggling to make sense of what happened, how vulnerable they felt, how unsupported – a lot of healing is needed.
“Apart from fearing for their own health, and taking Covid to their homes, the stigma that built up around Covid was fascinating and terrifying at the same time. Because very quickly people were like, well, we don’t really want to see you because you are working in a clinic, or you are working in a hospital and you are going to make us all sick. This reminded me of the early days of HIV – people not wanting to share cutlery or toilets, or sit on the bus next to somebody, you know?”
Working with the Department of Health
She highlights clinicians society’s role in advocacy and providing information to members. It has active social media platforms, hosts online conferences and regularly posts HIV and sexual health “best practice” guidelines on its website. It has also given clinicians advice on what to do when important antiretrovirals are out of stock.
“A lot of it is about communication and then often linking people up, helping them to know what systems are in place locally,” she says.
The society endeavours to work closely with the Department of Health.
Over the years, its guidelines have often been at the forefront of translating the latest scientific evidence on HIV into practical, evidence-based advice for the South African context.
“Obviously we produce our own guidelines on various elements of HIV and associated management,” she says. “We have academics from across South Africa, engaging in producing our guidelines, gathering the latest evidence on various elements of HIV and associated management. And often it’s very empowering for the Department of Health to have that, to see where we should be going.”
As an example, she cites the society’s gender-affirming healthcare guidelines – a 27-page document uploaded in October 2021.
“Particularly the gender-affirming guidelines are something completely new, so that will open up discussions across the country,” she says.
“So, for transgender and gender non-conforming communities in South Africa, as you might imagine, any services really are only available in the cities. And even in those cities, most of it is in private healthcare. So again, there’s an advocacy role about sensitising communities to not bully or threaten or refuse to care for people who are transgender or gender diverse. Such patients who attend rural clinics need to be treated with respect.
 “The medical bits were written by our academic experts in the field. I mean, it helps to explain why even hormone therapy should be available at primary level, really. You shouldn’t have to be referred to see an endocrinologist at a city hospital.”
“The medical bits were written by our academic experts in the field. I mean, it helps to explain why even hormone therapy should be available at primary level, really. You shouldn’t have to be referred to see an endocrinologist at a city hospital.”
Houghton explains that this is still the early stage for these particular guidelines and that the society is working on developing a short course on transgender and gender-diverse [TGD] patients for health workers across the private and public sectors. Ultimately, they hope the department will incorporate these and other guidelines into policy.
Important to laugh
During the interview, Houghton chuckles often. Speaking of her birth town of Warwick, she jokes: “Well, it’s famous for not much more than castles and it’s near Stratford-upon-Avon, the birthplace of Shakespeare. So that’s where my name comes from [Romeo and Juliet]. I guess I am lucky it’s not Titania [a character in Midsummer Night’s Dream] or something like that.”
Wrapping up, she says: “For me, laughter is a key mechanism to coping. Of course, it can be seen as entirely inappropriate for a health worker to laugh because we could be seen to be laughing at things that aren’t funny at all.”
She shrugs, adding: “But I like to laugh. And I think, you know, it’s healthy.”
* This article is the first in Spotlight’s 2022 Women in Health series that will run throughout August. The series celebrates and highlights the contributions to health and science made by women in South Africa.
*This article was published by Spotlight – health journalism in the public interest.




















Comments - Please login in order to comment.