Maverick Citizen Op-Ed
Dexamethasone is not the Covid-19 ‘silver bullet’ we are looking for
While the world waits for a Covid-19 vaccine, scientists are also urgently looking for medicines to help manage and mitigate the virus’s severe health effects. What should we make of the latest sliver of hope?
With confirmed Covid-19 cases worldwide surpassing 9.9 million and continuing to grow, scientists are pushing forward with efforts to develop vaccines and treatments to slow the pandemic and lessen the disease’s damage. From a medical perspective, the development of a vaccine is seen as the only intervention that can provide a longer-term solution to the problem, as the virus spreads easily and the majority of the world’s population is still vulnerable to it.
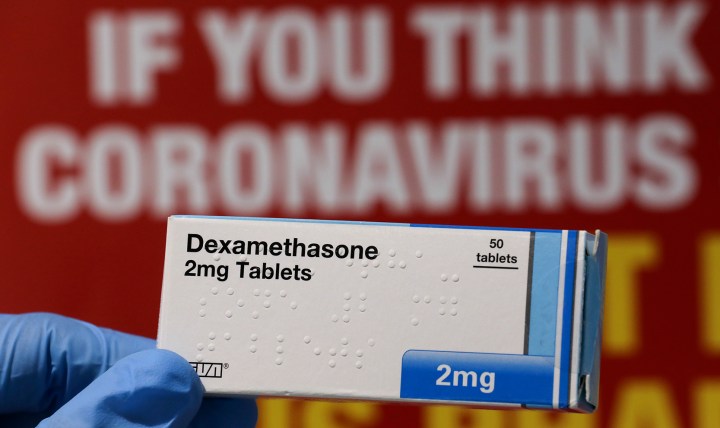
But a desperate search is also on for medicines to help already sick people fight the virus. On 19 June South Africa’s Minister of Health Dr Zweli Mkhize announced that the Department of Health, on advice of the Ministerial Advisory Committee on Covid-19, had approved the use of the drug dexamethasone for all Covid-19 patients on ventilators or requiring non-invasive supplementary oxygen.
This led to a dramatic increase in demand for the drug, with local suppliers reporting they had run out of stock. The minister’s policy decision and announcement should, ideally, have been preceded by a thorough assessment process that considered the medical, social, economic and ethical issues related to the use of the drug in a systematic, transparent, unbiased and robust manner. While the broader context of the public health emergency facing the country makes the haste with which the announcement was made understandable, we must ask: Is dexamethasone a “silver bullet” or another “false dawn” in the search for medication to combat Covid-19?
Context and false dawns
The minister’s announcement must be seen within the context of South Africa entering the “take-off” phase of the pandemic, with a rapid increase in the number of cases as the lockdown is progressively eased. Based on a Mail and Guardian survey, there will be a nationwide shortage of the staff, equipment and facilities needed to cope with the number of infected people set to flood the healthcare system when the outbreak hits its peak.
The announcement of an effective treatment holds the promise of not only saving lives, but also a justification for some lockdown measures to be lifted more quickly. Having an effective treatment would reduce the impact of the coronavirus on people’s health and the health system’s resources. If it stopped patients admitted to hospital from needing ventilation, there would be less risk of intensive care units being overwhelmed, so controls of people’s lives may not need to be as strict.
However, in the search for drugs to help manage the epidemic, there have been a number of “false dawns”. Donald Trump’s now-infamous promotion of hydroxychloroquine is a case in point.
There has been much talk, but little evidence, that a pair of HIV drugs – lopinavir and ritonavir – would be effective in treating the coronavirus.
Hopes in South Africa were high that the BCG tuberculosis vaccination would have an impact on Covid-19 morbidity and mortality. However, leading experts from the Vaccines for Africa Initiative and the South African TB Vaccine Initiative at UCT have concluded that “there is no evidence to indicate that BCG vaccination is safe in older populations”. If we are to consider using BCG in the Covid-19 pandemic in South Africa, then this first needs to be subjected to a clinical trial to generate evidence.
Is dexamethasone another of these “false dawns”?
Medical considerations
Excitement about dexamethasone as a medicine to assist in the treatment of Covid-19 is based on findings of the Randomised Evaluation of Covid-19 Therapy (RECOVERY) trial. The study was carried out by researchers at the University of Oxford in the UK. In the study, a total of 2,104 patients were randomised to receive dexamethasone and were compared with 4,321 patients who received “usual care” alone.
Dexamethasone reduced deaths by one third in ventilated patients and by one fifth in other patients receiving oxygen only. There was no benefit among patients who did not require respiratory support. Given the strength of the results, dexamethasone has been widely labelled as a “breakthrough” in Covid-19 treatment. As convincing as the results of the study appear to be, the results of the RECOVERY trial have not yet been published in a peer-reviewed journal. The website indicates: “Given the public health importance of these results, we are now working to publish the full details as soon as possible.”
The question then is whether we should be proceeding based on the provisional findings of a single study carried out on a population that is very different from ours? Experts locally appear to have given a qualified green light based on the following:
First, there are grounds for the provisional results to be immediately translated into clinical practice, given the nature and severity of the public health emergency in which there is no other proven effective treatment.
Second, the research has a number of strengths. It was carried out by credible researchers, the study was a well-designed randomised controlled trial with a publicly available protocol and transparent data collection processes, the sample size was large, the study design rigorous, and the magnitude of the impact of dexamethasone is large.
Social and economic considerations
Assuming that dexamethasone is as effective as claimed, does the approval of the drug make broader social and economic sense? Dexamethasone is a cheap, locally produced steroid and it should be feasible to meet local demand. In his announcement, the minister said it would be easy to implement use of the medicine since it was inexpensive, easy to transport, easy to administer and would not require additional training. Health workers in the country are familiar with the drug, having used it for years as a registered medicine in South Africa.
However, spending money on a drug because it is cheap does not necessarily imply a good use of limited resources. The net costs, relative to the clinical risks and benefits, also need to be considered in deciding whether this drug is a good investment relative to other potential health investments. A cost-effectiveness analysis carried by MOSAIC (a health economic modelling collective) investigated how effective dexamethasone is compared to how much it costs. The analysis found dexamethasone to be highly cost-effective with an incremental cost of R552 per disability life year (DALY). Any intervention with a cost of less than R38,465 per DALY averted is likely to be a good investment for the South African public health sector.
While dexamethasone is expected to be a cost-effective intervention, it is administered to hospitalised patients and so a key issue remains the likely shortage of both ICU and general ward beds, particularly in the public health system. In earlier work, MOSAIC found that ICU care itself is not cost-effective. This result is driven by the high costs and poor outcomes of ICU care, at a cost per admission of approximately R165,000, with 54% of patients dying.
Given that it is expected to reduce deaths in ventilated patients and patients receiving oxygen, does dexamethasone make ICU care cost effective? MOSAIC updated its previous ICU analysis to include dexamethasone and estimated the incremental cost of ICU care to be R70,399 per DALY averted. While dexamethasone improved the cost-effectiveness of ICU care, the improvement was not enough to make ICU care cost-effective. Only if dexamethasone averts 90% of ICU deaths does ICU become reasonably cost effective.
Conclusion
Based on the available evidence, dexamethasone could assist in reducing deaths among ventilated patients and patients receiving oxygen, but this needs to be confirmed for the South African context.
Dexamethasone is likely to represent a good use of limited health resources not because it is inexpensive but because its net costs, relative to its clinical risks and benefits, make it a good investment relative to other potential health investments. If effective as claimed, it would improve the cost-effectiveness of ICU care but not to the extent that ICU care is cost effective. While dexamethasone is a welcome addition to the “toolkit” for managing the epidemic, it is not the magic bullet we are desperately looking for. DM/MC
Geetesh Solanki is specialist scientist at the Health Systems Research Unit, SA Medical Research Council and an honorary research associate at the Health Economics Unit, University of Cape Town. Tommy Wilkinson writes in his capacity as a researcher at the Health Economics Unit, University of Cape Town. Cynthia Tamandjou Tchuem is a virologist and researcher at the Health Economics Unit, University of Cape Town. Sumaiyah Docrat is a health economist at the Alan J Fisher Centre for Public Mental Health, University of Cape Town. Emmanuelle Daviaud is a specialist scientist at the Health Systems Research Unit, SA Medical Research Council. Susan Cleary is an associate professor at the Health Economics Unit, University of Cape Town.
The opinions expressed here are those of the authors and do not necessarily reflect the views of their institutions.
"Information pertaining to Covid-19, vaccines, how to control the spread of the virus and potential treatments is ever-changing. Under the South African Disaster Management Act Regulation 11(5)(c) it is prohibited to publish information through any medium with the intention to deceive people on government measures to address COVID-19. We are therefore disabling the comment section on this article in order to protect both the commenting member and ourselves from potential liability. Should you have additional information that you think we should know, please email [email protected]"





 Become an Insider
Become an Insider