/file/dailymaverick/wp-content/uploads/2025/09/label-Opinion.jpg)
South Africa faces the reality of serious skills shortages in healthcare. There are many reasons, which need no repetition here. What needs more attention is the parallel reality unfolding quietly alongside it. This is the rich reservoir of senior clinical expertise which is being relegated to lie dormant at the very moment when the system’s demand for judgement, continuity and mentorship is intensifying.
This article proposes strategic recourse to this pool. It attempts to raise a national stewardship issue between productive citizens and the government, what I call “shared stewardship”.
Across the country there is a growing cohort of senior clinicians whose professional lives span decades of patient care, crisis navigation, institutional leadership and the development of younger clinicians of all disciplines. Their experience is more than just the volume of service historically rendered, but includes judgement under pressure, ethical tensions and travails, and tacit knowledge that cannot be replicated through protocols or accelerated training.
Much of this expertise unwillingly exits the system rather abruptly, under prescriptive legislation informed by linear thinking. Their capacity does not vanish. Their potential and relevance never expired. Instead, we have just failed as a country, over the years, to design a coherent pathway through which accumulated wisdom can continue to serve beyond formal retirement thresholds.
Healthcare systems advance through more than numerical staffing levels. The value of head count and doctor-patient ratios lies in what might be called the clinical expertise-disease burden coefficient. The challenge extends beyond staff shortages. The deeper question lies elsewhere. It is in how much experiential and tacit judgement-bearing clinical intelligence exists relative to the complexity and severity of the disease burden facing the nation.
This hypothetical coefficient would improve most reliably through intentional intergenerational transfer. Its advances will lie in experienced clinicians remaining in sustained professional proximity to those still developing and maturing into strategic leadership “beyond the stethoscope”. Such transfer is neither automatic nor accelerated by qualification alone. It requires a culture of clinical rites of passage, where maturity is cultivated, recognised and entrusted through lived practice, rather than being presumed on the basis of technical credentials alone.
This call to fellow senior clinicians reaches deeper than merely motivating for institutional rescue. It is an invitation into an intentional cycle of national stewardship, rooted in legacy formation rather than contract. It speaks to honour, continuity and responsibility, before any consideration for remuneration.
Protecting and transmitting knowledge
This responsibility does not rest on personal preference. It is embedded in the logic of life itself. Every enduring species survives by protecting and transmitting its most adaptive knowledge across generations, each generation nurturing and safeguarding the next.
Healthcare is no exception.
When lived clinical wisdom is not carried forward deliberately and consistently, continuity is disrupted and vulnerability escalates.
Modern economies already extract from the future through debt-based development. Health systems compound this extraction when they discard mature reservoirs of clinical skill even as disease complexity intensifies. The deficit burden migrates forward, re-emerging as avoidable error, clinician burnout, ethical erosion and systemic fragility in the next generation. It will not disappear.
A proposal for shared stewardship
Some existing service delivery frameworks already demonstrate that flexible, wisdom-centred deployment of senior clinical expertise is feasible. Credit is due. The District Clinical Specialist Team model illustrates one possible pathway for structured recourse to senior judgement, without prescribing it as a single or rigid design.
Senior clinicians, many of whom have secured stable pensions, should reasonably consider in patriotic conscience, service at reduced remuneration, even at 50% of legislated rates. The Occupational Specific Dispensation was crafted without adequate regard for long-term fiscal projections. It need not remain the country’s albatross.
Stewardship is an expression of personal maturity. It is obedience to the burden of privilege. The question is no longer whether the country can afford to rethink its relationship with senior clinical wisdom. The question is whether the country can afford not to. It is not impossible.
Caution must be raised, that the responsibility does not lie with the state alone. It calls for a mutual covenant. It rises above any abdication by government or romantic voluntarism by citizens. It calls for shared stewardship, as it must be, if the country is to be saved from implosion, and even as humanity itself globally needs it to stem its looming moral and ethical vortex.
States cannot carry continuity alone. Citizens cannot outsource moral responsibility to institutions without consequence. Civilisations endure only when responsibility is distributed relationally across generations, professions and social strata.
When stewardship collapses into entitlement or a monetised value proposition, systems hollow out. What will follow will never be a sudden catastrophe, but a slow implosion, as we are currently witnessing. DM
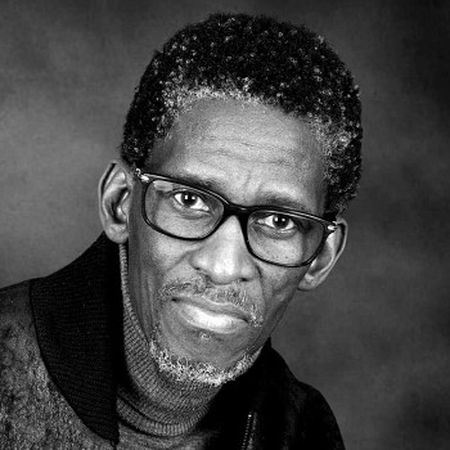
Dr Zolile Mlisana is a paediatrician whose work spans clinical practice, institutional leadership and public-interest thought leadership. He recently retired from public service at the prescribed age of 65 and has since returned to private practice. He is a former founding chairperson of the South African Medical Association and former principal of Medunsa.