VACCINE PATENTS OP-ED
None are safe until everyone is: Why poor economics kills

The world is being failed by an unfair system upheld by a few rich countries. Its poorest citizens in particular are being held to ransom by an international system of intellectual property rights that serves only to protect big pharmaceutical companies’ patents and exorbitant profits.
The knowledge recipe necessary to make Covid-19 vaccines accessible is being prohibited from use through a system of patents. Millions of people will die unnecessarily as a result.
The profiteering from vaccine inequity is serious enough to have been described in the British Medical Journal as a crime against humanity.
Flimsy arguments on the “economics of innovation” are being deployed to justify the current patent system. Economic myths around Covid-19 vaccines are being used to block the proposal for a waiver of the Trade-Related aspects of Intellectual Property Rights (Trips) at the World Trade Organization (WTO) for life-saving vaccines. We urgently need, in the short term at least, a waiver of Trips for pandemic-related vaccines and therapeutics.
Beyond the waiver, it has become crystal clear that the world needs an effective international institution to champion collaboration over desolation. This means building the international organisations that make life-saving medication and technology a global public good. From discovery to access.

Indonesian activists hold a banner during a protest in front of the Swiss Embassy in Jakarta on 30 November 2021 to urge Switzerland, the EU and the UK to agree on the Trips waiver proposal, which will encourage wider vaccine production to provide equitable access to vaccines in developing countries. (Photo: EPA-EFE / Bagus Indahono)
Most countries around the world have slowly come to realise, the very hard way, that protecting Big Pharma’s intellectual property only increases its profit thereby making the world more unequal and less safe socially, health-wise, politically and economically. Only the European Commission, the United Kingdom, Germany, Switzerland and Norway still oppose the Trips waiver, essentially protecting undeserved profits over protecting humanity and basic human rights.
According to Oxfam, nine new billionaires emerged from vaccine profits. Big Pharma’s Moderna, Pfizer and BioNTech have made a combined pre-tax profit of $34-billion in 2020.
In their campaign to oppose the Trips waiver, Big Pharma and the countries protecting it have been using myths around innovation and productive capacity. These are mostly red herrings. Most of the arguments used are misleading and lack the constructive thinking necessary for urgent global vaccine access. It is possible to incentivise the innovation of vaccines globally without allowing Big Pharma and the most powerful countries to profit off of the hardship of a pandemic.
To understand why, we must first dissect the distractions.
Myth #1: Innovation is only driven by profits, patents, and corporate interests
One myth is that the creation of new vaccines will halt if private companies are not able to make profits from them.
In the case of the Covid-19 pandemic crisis, this does not hold water. The majority of funding that incentivised vaccine technology innovation was derived from taxpayers’ pockets. Taxpayers supply governments with the funds to pay for a range of social goods, including research and development (R&D) that incentivise innovation. Estimates of direct public spending by the US government on the development and manufacturing of Covid-19 vaccines range between $18-billion and $39.5-billion.
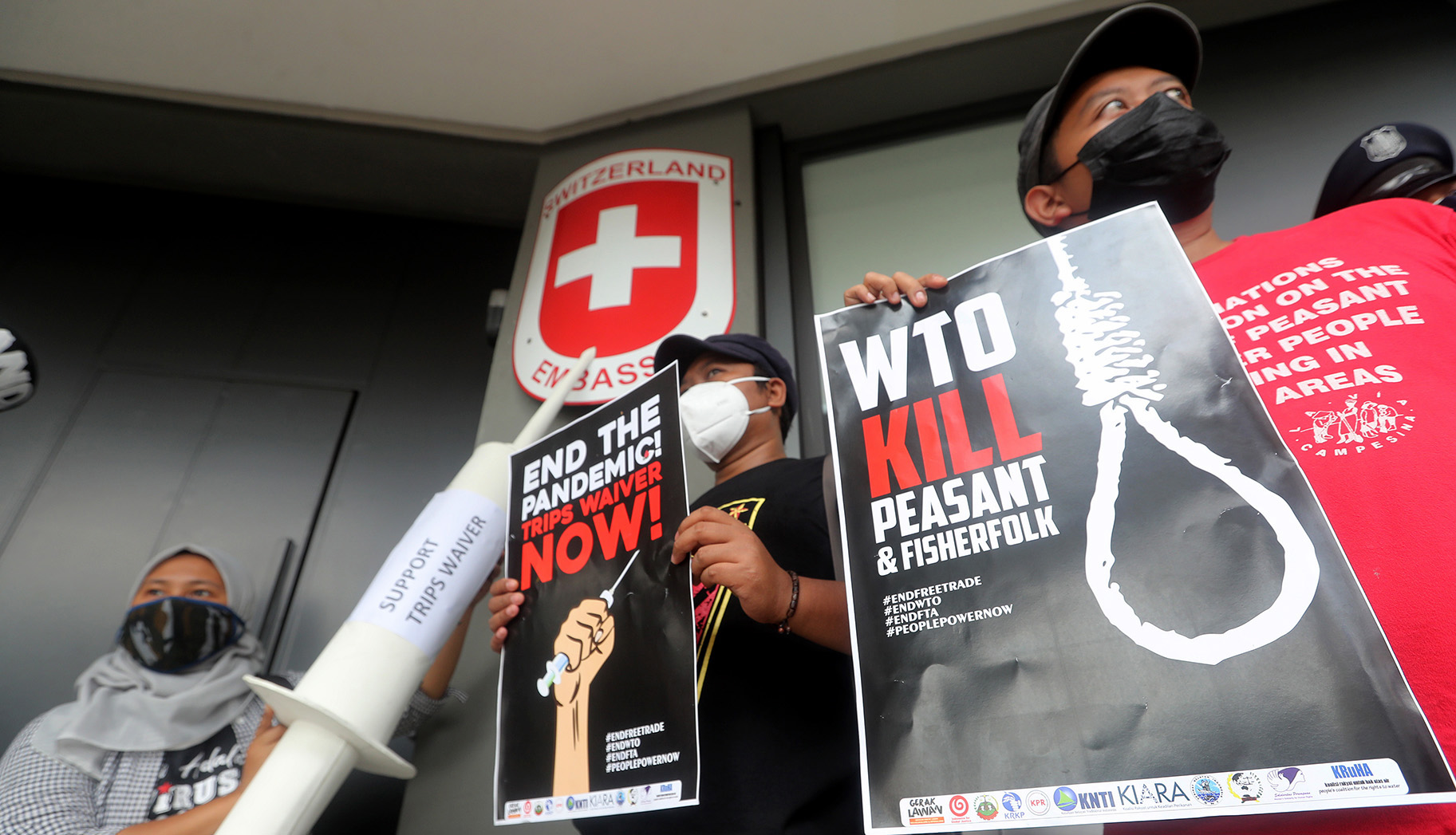
Indonesian activists hold a banner during a protest in front of the Swiss Embassy in Jakarta on 30 November 2021 to urge Switzerland, the EU and the UK to agree on the Trips waiver proposal, which will encourage wider vaccine production to provide equitable access to vaccines in developing countries. (Photo: EPA-EFE / Bagus Indahono)
Innovation is the process of creating a new process or product, incentivised by what economists might call “push” and “pull” incentives. Push incentives are the basic inputs that lay the ground for building up ideas and formulas. These include R&D grants to research laboratories and to universities that pay for research projects into things like vaccine innovation. These push incentives come before an invention is made and commercialised. Mostly, this comes from the government and universities. According to our calculations, based on Organisation for Economic Co-operation and Development (OECD) data, the combined spending on all R&D from government and universities by the UK, Germany and Switzerland is estimated to be about €205-billion in 2019.
Pull incentives, on the other hand, offer the promise of profit after an invention is made.
Patents are the most common pull incentives. Firms that patent an invention can make monopoly profits by excluding others from using their product or process for a period of time. Legal patents are the incentive that pulls them towards innovating because they will get legal protection to be the only ones able to produce a good.
But in the Covid-19 pandemic, the pull incentive for pharmaceuticals came mostly from the governments of rich countries. This took the form of the Advance Purchase Mechanism (APM) whereby rich countries promised to buy large quantities of the vaccines from the pharmaceutical companies if they successfully created one. This promise reduced innovation risks because the demand was guaranteed to cover the costs of the invention process.
Over the past two years, vaccines were incentivised by taxpayer money and the monopoly power was still given to Big Pharma through patents as incentives that they did not even need. In the end, we have somehow allowed Big Pharma to profit from an international disaster that it has failed to resolve. You are not alone in feeling that you have been swindled by the biggest international scam of our time.
This is especially tragic because the international community is capable of creating a common resource pool to incentivise vaccine innovation in the context of a pandemic.

People stand in front of empty chairs arranged to form the number ‘10,000’, as the number of daily casualties due to Covid-19 are displayed at the United Nations in Geneva during a demonstration on 30 November 2021 for an intellectual property rights waiver for Covid-19 vaccines and supplies. (Photo: EPA-EFE / Salvatore di Nolfi)
Myth #2: Developing countries cannot produce their own vaccines
The second myth being spread is that the patent waiver will not solve the global shortfall of vaccine production because developing countries do not have the capacity to produce them.
This is a deceptive argument. It is true that the Trips agreement is only one of the barriers to global access. While there are others, most can be overcome.
In the end, if the patents are not the problem, then why not just waive the patents? It is simply not true that there is not enough capacity in developing countries to produce enough vaccines to meet global demand.
India alone manufactured 60% of the world’s vaccines before the pandemic. If pharmaceutical companies in the Global South were given access to the knowledge protected by patents and the necessary technology transfer, they would have been competent to manufacture Covid-19 vaccines and contribute to global demand.
In fact, there are at least 120 manufacturers in the Global South capable of vaccine production, including in South Africa, India, Pakistan, Bangladesh, Indonesia, Senegal, Argentina and Brazil. Some economists estimated that by the end of 2021, we could have vaccinated the world’s population. The vaccine scarcity we face is artificial and created in the interests of protecting profits for a few rich countries and Big pharma.
Myth #3: Global vaccine demand can be met through charity
Other arguments against the Trips waiver are simply attempts to distract and deceive. These include stories of how voluntary licensing measures and the WHO’s vaccine sharing mechanism (Covax) are enough to fill the massive gap in the current system. Our reality is the evidence: as much as 98% of people in low-income countries remain unvaccinated with Covax contributing less than 5% of all vaccines administered globally.
Mechanisms of sharing vaccines and the knowledge to produce vaccines have obviously not worked out. Mostly, because they rely on charity instead of on institutionalised solidarity. Meeting global vaccine demand urgently and equitably needs cooperation in accountable international organisations. Reliance on donations must be replaced by a new system of health innovation, as outlined next.
A new system of health innovation
Young people are being failed by the current generation of leaders who make and support these arguments built on sand. It is disappointing to watch them fail to build concrete and long-term solutions. The voices of legal experts, civil society and students demanding a system that is both innovative and fair should be amplified.
The failure to have a truly international response to the pandemic has resulted in a tragedy of our international health commons. Governments, especially the rich ones, have chosen their short term self-interest at the expense of a long-term international solution that could make everyone better off. Vaccine hoarding, jumping the queue for the WHO Covax project and especially the use of patents to prevent the developing world from producing its own vaccines have made everyone worse off.

People hold placards in front of Campus Biotech in Geneva on 30 November 2021 during a demonstration for an intellectual property rights waiver for Covid-19 vaccines and supplies. (Photo: EPA-EFE / Salvatore di Nolfi)
Ultimately, such alternatives exist, but are being ignored. The international community is more than capable of building institutions that use a combination of push and pull incentives to create a global commons for critical health technologies.
For instance, a common resource pool could be established to which countries would contribute a portion of their national budgets proportional to their income and population size. This resource pool would then be used to strategically incentivise research and development. It can also be used to buy or replace patents for key inventions by offering other pull incentives such as advance purchase commitments, pooling and prizes.
Such an institution’s goal would be to keep the price of life-saving technology low and keep access equitable — all the while greasing the wheels of innovation. As eloquently put by Suzanne Scotchmer, “Progress is limited by human imagination, and in some historical periods or geographic locations, by an inability or unwillingness to marshal resources.”
Looking forward, we do not need to be stuck by the institutions that exist, nor by the ones that we are yet to create. DM/MC
Kamal Ramburuth-Hurt, Kristin Dilani Nadaraja and Joao Braga are from South Africa, Norway and Brazil respectively. The authors are pursuing masters degrees in Economic Policies for the Global Transition (EPOG) in Paris. The authors are part of the international Rethinking Economics movement that aims to make economics more critical, pluralist and applied to real-world problems. For queries contact [email protected]
Key References
Gosh, J. 2021. Nobody is Safe if Someone is Unsafe. Institute for New Economic Thinking. A dialogue between Jayati Ghosh, Rohinton Medhora, Joseph E. Stiglitz, coordinated by Robert Johnson at the 2021 Trento Economics Festival, 17 June 2021.
INET. 2021. The Pandemic and the Economic Crisis: A Global Agenda for Urgent Action. Institute for New Economic Thinking.
Kremer, M. and Glennerster, R., 2004. Strong medicine: creating incentives for pharmaceutical research on neglected diseases. Princeton University Press.
Scotchmer, S., 2004. Innovation and incentives. MIT press.
[hearken id=”daily-maverick/8976″]
"Information pertaining to Covid-19, vaccines, how to control the spread of the virus and potential treatments is ever-changing. Under the South African Disaster Management Act Regulation 11(5)(c) it is prohibited to publish information through any medium with the intention to deceive people on government measures to address COVID-19. We are therefore disabling the comment section on this article in order to protect both the commenting member and ourselves from potential liability. Should you have additional information that you think we should know, please email [email protected]"





 Become an Insider
Become an Insider