SPOTLIGHT
Bringing it home: Khayelitsha project shows how a focus on family can boost TB prevention

Tuberculosis preventive therapy is highly effective in preventing TB disease and death, yet only a few people have access to it. Tiyese Jeranji reports on how Médecins Sans Frontières in Khayelitsha is helping TB patients and their contacts access preventive therapy in the comfort of their homes as part of a new family-centred care initiative.
Tucked away outside Cape Town, Khayelitsha is home to about half a million people. Many families in the sprawling yet congested area share small corrugated iron houses with limited access to basic services such as clean water and sanitation. It is in areas like these that diseases such as tuberculosis (TB) spread rapidly.
According to Dr Anja Reuter from Doctors without Borders (MSF), there are about 170 to 200 cases of rifampicin-resistant tuberculosis (RR-TB) per year in this area, with 70% co-infected with HIV. Rifampicin is a key drug in the treatment of drug-susceptible forms of TB. When people are resistant to it, they have to be treated with drugs with a less favourable side effect profile than the standard ones. Resistant strains of TB can be transmitted from one person to another.
Working with the department of health in the province, MSF is trying to ensure that people with RR-TB in Khayelitsha are started on treatment as soon as possible. They are, however, taking it a step further by testing the household contacts of people with RR-TB and treating those who test positive. They also offer TB preventive therapy to those who do not test positive, focusing mainly on family members who are 19 years old or younger. They are trialling a model of family-centred TB treatment and care.
A saving grace
For Nonki*, the MSF programme has been a saving grace. Her brother fell ill in the Eastern Cape and his mother said he must come to Khayelitsha to be with his other family members.
“We took him to the hospital, but because he didn’t have a file at a nearby clinic, they took time to help him. At that time we didn’t know what to do because we were staying in this tiny house… we slept together. We shared everything. That was not long before I started getting sick. I felt weak and slept the whole day. I was sweating at night. I decided to go to the clinic. They did the screenings and ran some tests on me. After that they told me that I have MDR-TB,” she says. (MDR-TB is TB that is resistant to both rifampicin and isoniazid, although the term is sometimes used interchangeably with RR-TB.)

The number of people who were provided with TB preventive therapy globally increased from 1.0 million in 2015 to 3.6 million in 2019, but this positive trend was reversed in 2020 when it fell back to 2.8 million. (Photo: Gallo Images / Foto24 / Lulama Zenzile)
She says she realised she shouldn’t hide the fact that they were staying with children, as they might also have contracted the disease. “I told them (at the clinic) that at home we are many, and there are children. So they were also called and were tested. Some were diagnosed with TB. That is when they started taking treatment. It was found that my mother, my older child, and my younger brother did not contract TB, so they were put on preventive medication,” she says.
Her mother says they had a poor understanding of MDR-TB. “I was shocked because many people with this TB were dying, even transferred to the hospital in Brooklyn Chest Hospital. So, here at home, it was devastating since we lost a family member because of TB. But the more the nurses came, we understood the disease and we understood that it was curable,” she says.
She says that what kept them going was the support they received from the multidisciplinary team who came to their house to support them. “They just didn’t come for TB issues… they checked if we’re doing okay, if we had food. The kids were getting groceries. They know our situation in this family. We sometimes see either a social worker bringing a food parcel… last week they bought tekkies for the kids because they know the situation at my house. This has really helped us to deal with TB and for that we are grateful,” she says.
A holistic family-centred approach
Reuter says understanding the family within the home environment is key in offering family-friendly services for RR-TB. “Family-friendly care includes preventative and curative TB services for the whole family. Through this model, it allowed us to holistically care for the whole family in a community setting,” she says.
Erika Mohr-Holland, DR-TB Epidemiology Activity Manager at MSF, explains that the family-centred approach includes providing holistic care for the family rather than just treating the index case for RR-TB.
“Providing care at the household level enabled us to get a better understanding of the family composition and needs (socio-economic/social) and to identify more contacts that would benefit from TB preventive therapy. Additionally, we were able to detect child/adolescent contacts with RR-TB disease and get them on treatment sooner,” she says.
Mohr-Holland thinks the approach is excellent as it has ensured the provision of more holistic, family-centred care in which not only treatment of disease was provided, but the whole family was assessed as a unit. The care provided was differentiated based on the identified needs of the individuals in the family – such as the detection of diseases other than TB, the need for TB preventive therapy, social support and counselling that can be tailored to the needs of children. The home-based care service was provided by multi-disciplinary teams consisting of a nurse, a doctor, a patient support manager, a social worker and a peer supporter.
Focus on prevention
According to the World Health Organisation’s Global Tuberculosis Report 2021, the main healthcare intervention available to reduce the risk of TB infection progressing to active TB disease is preventive therapy. Until recently, preventive therapy involved taking an isoniazid pill every day for at least six months, but three-month and one-month alternatives are also becoming available. Spotlight previously reported on the introduction of 3HP in South Africa – a three-month preventive therapy regimen consisting of the drugs isoniazid and rifapentine.
The number of people who were provided with TB preventive therapy globally increased from 1.0 million in 2015 to 3.6 million in 2019, but this positive trend was reversed in 2020 when it fell back to 2.8 million.
The WHO estimates that in 2020, 93% of people living with HIV in South Africa, newly started on antiretroviral therapy, were also started on preventive therapy for TB. The picture is less positive when it comes to children, with only an estimated 51% of under-fives who live in households where someone has been diagnosed with TB having been started on preventive therapy.
From March 2020 to August 2021, the MSF programme in Khayelitsha identified 150 contacts of people with RR-TB for post-exposure management. Two of the contacts had drug-sensitive TB, 13 had drug-resistant TB, and 135 contacts were potentially eligible for preventive therapy – although only 119 actually started taking it.
Of the 119, 61 have so far completed preventive therapy, 45 are still on it, 11 were lost to follow-up, one was referred to another study and two discontinued preventive therapy due to an adverse event.
Screening kids in their homes
The home-based, family-centred approach builds on previous research conducted by MSF. In 2017, MSF launched a pilot programme in Khayelitsha that set out to screen for TB and follow up adolescents and children who had been exposed to drug-resistant TB in their households so that they would be able to respond quickly if these individuals did in fact develop the disease.
Mohr-Holland says in 2017 there was no preventive therapy for children (guidelines did not provide for it) so the model entailed screening contacts and following them for a period of two years, doing more routine screenings to see if they developed TB disease, and if they did, to link them to treatment as soon as possible.
“This model did not incorporate the home-based care approach and thus there were many barriers in accessing care at the facilities [for example] getting to the facility when already under economic strain (money for transport, missing work or school to be screened), being seen in a timely manner at the facility (long wait times, no fast-tracking of healthy kids), and no preventive therapy,” she says.
However, in 2019, South Africa’s RR-TB treatment guidelines were updated, recommending RR-TB preventive therapy for certain high-risk individuals, including household contacts. Additionally, due to Covid, the model of care was adapted to provide home-based care and telephonic follow-up for some contacts initiated on preventive therapy.
“Bringing care closer to the community, with a model that allowed for more flexible follow-up and multi-month dispensing of preventive therapy, meant that the families were not as strained by being required to go to the facilities for screening, preventive therapy initiation, and follow-up,” she says.
Presenting the initiative at the recently held 52nd Union World Conference on Lung Health, MSF DR-TB nurse, Ivy Apolisi said there are gaps in the diagnosis of children and adolescents; one of the reasons is that the current model of care is not friendly to children and their caregivers.
“Due to Covid-19 we modified our post-exposure management and the modification included home visits and screening kids in their households. During home or clinic visits the basic assessment included clinical assessment and TB symptom screening for all, and chest X-ray and Xpert MTB/RIF testing at the discretion of the clinician if there was a presumption of TB disease.
“Diagnosis was made on the basis of these findings. Children who were diagnosed with TB were started on TB treatment immediately in the community,” she says. If TB disease was ruled out, the child was started on a six-month course of TB preventive therapy with isoniazid. (Xpert MTB/RIF is the gold standard molecular test with which TB is currently being diagnosed in South Africa.)
Apolisi says they identified DR-TB champions from local clinics and trained them on how to diagnose and manage children in the local clinics. “This allowed for early diagnosis of mild disease. These kids were provided child-friendly injectable-free regimens because we had access to child-friendly formulations. Through this model and the post-exposure management protocol, there has been a drastic increase in case detection.
“The rate of co-prevalent TB detection via the post-exposure management programme was higher than that reported in the existing literature. Many paediatric cases go undetected in this population and Covid has further exacerbated gaps in the cascade of care,” she said, adding that not all children and adolescents’ contacts diagnosed with co-prevalent TB disease had symptoms of TB, highlighting the poor sensitivity of the existing screening tools and the need for robust clinical evaluation.
Successes and challenges
Presenting at the same conference, Mohr-Holland said that preventive therapy is imperative in reducing the risks of morbidity and mortality associated with RR-TB.
“We are very far from reaching our target of 30 million people on preventive therapy by 2022… we are currently at 6.3 million people (this is a multi-year figure, which is why it is higher than the WHO figures quoted earlier).
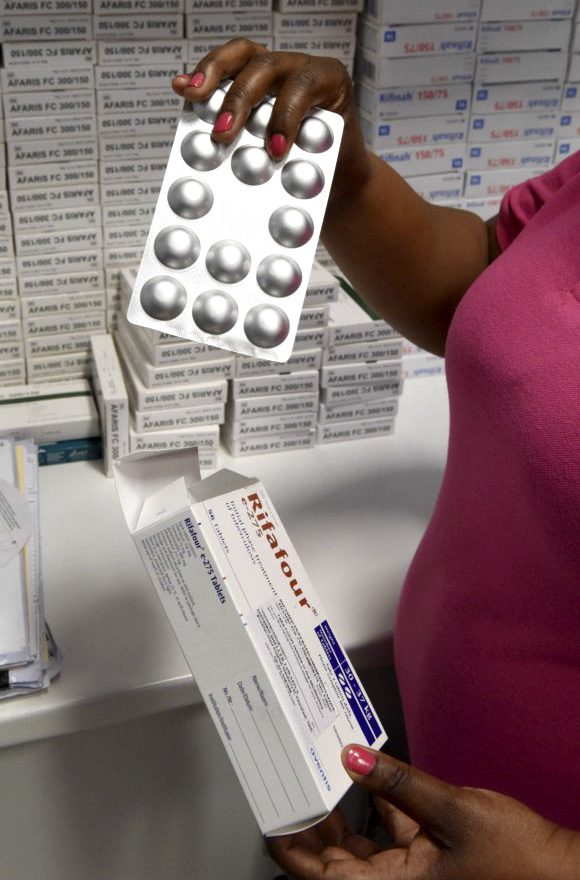
Tuberculosis medication at Site B Community Health Centre in Khayelitsha. (Photo: Nasief Manie / Spotlight)
“In Khayelitsha, the preventive therapy roll-out has been successful as families have been accepting of preventive therapy and there has even been demand for preventive therapy due to concerns about the risks posed by Covid on TB transmission.
Additionally, the lockdown and school closures made it easier to interact with the population of interest, highlighting the importance of differentiated models of care to engage with this population,” she said, adding that traditionally post-exposure management services are offered at clinics. However, with the home-based care model, this meant fewer visits to the clinic, thereby saving patients money and time.
As with any successful programme, Mohr-Holland said there were challenges.
“There was trouble reaching families with no cell phones or incorrect numbers, meaning they had to be followed up post-preventive therapy initiation at the household or clinic. At the onset of the Covid-19 pandemic, when the home-based care team arrived at patients’ households wearing scrubs, it further perpetuated stigma associated with Covid in the community. Thus, we had to change our attire and think about what we wore when conducting home visits,” she says.
“Additionally, unfortunately, Khayelitsha has a high rate of violent crime so individuals living in areas with safety concerns would have to be seen at the clinic or followed up telephonically.”
Can it be scaled up?
At the moment, Mohr-Holland says they are working with stakeholders on better capacitating community healthcare workers (CHWs) to provide these home-based services. The proposal is to train and mentor CHWs to feel better equipped to provide post-exposure management services, conduct household-level TB screening, and provide follow-up support to families in which there are people on preventive therapy.
“The aim is that CHWs could be involved in conducting household assessments, including screening of household contacts and then providing routine follow-up and support to individuals started on preventive therapy, linking them to care should medical care be needed for adverse events due to preventive therapy (which are uncommon and mild).
“This proposal is still in the development phase — MSF is busy in conversations with the city and provincial departments of health and the various different stakeholders to refine the implementation plan, which will hopefully be piloted soon,” she says.
“We hope that this differentiated model of family-centred care for providing post-exposure management and TPT will be rolled out more broadly across the country.” DM/MC
* Not her real name.
This article was produced by Spotlight – health journalism in the public interest.





















 Become an Insider
Become an Insider
Comments - Please login in order to comment.