SPOTLIGHT IN-DEPTH
Gender-affirming surgery little more than a distant dream for the many hamstrung by high costs and long waiting lists
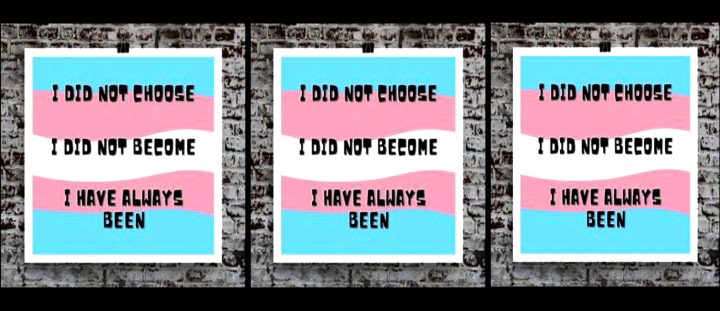
Already very long waiting times for gender-affirming surgery in South Africa’s public sector are now even longer due to the Covid-19 pandemic. Tiyese Jeranji investigates the challenges transgender persons in South Africa face in accessing gender-affirming care.
In South Africa, gender-affirming care is mostly only available in the big urban centres of provinces such as Gauteng, the Western Cape, KwaZulu-Natal, and the Eastern Cape.
Transgender people from rural areas or provinces where gender-affirming care is not available must travel long distances to the major cities to access these services.
“There are huge waiting lists and a scarcity of surgical expertise in South Africa. In the private sector, it costs hundreds of thousands of rands while in the public sector, waiting periods are often quoted as being north of two and a half decades,” says Dr Anastacia Tomson, an author and activist focusing on queer and transgender rights.
Dr Kevin Adams, a consultant plastic surgeon who also works at Groote Schuur Hospital, confirms that the waiting list for gender-affirming surgery is inordinately long.
“The Covid-19 pandemic has meant that we have been unable to do these operations for 18 months,” says Adams. The waiting list for surgery is over 300 patients long and as one operation can take a day, this means that there is a very long waiting list. We do not decide which surgery are permitted, but the vast majority of patients want at least one operation. Since the service was started in 2009, the number of patients entering the service has increased exponentially,” he says.
In 2009, Adams says they were seeing four to five new patients every three months and at the beginning of 2020, the number had doubled.
“There has been no increase in the amount of operating time as the service has increased, and therefore the waiting list continues to grow. There is only one surgeon performing these operations at Groote Schuur,” he says.
Dr Simon Pickstone-Taylor is a Child and Adolescent Psychiatrist, and General Adult Psychiatrist. Pickstone-Taylor, who set up the Gender Identity Development Services (Gids) within the Division of Child and Adolescent Psychiatry at Red Cross Hospital, says the waiting list is generally 25 years for youth and or adults.
“They (trans teens) are on the same list (with adults). Their starting date is when they first consult the Gender Identity Development Service. None of the youth has had top surgery on the state list to date. All those who have had top (or bottom surgery) have had it with parental finance and a very few with medical insurance paying. The state only allows very limited funding for these surgeries, thus the long waiting list,” says Pickstone-Taylor. (Top surgery refers to surgery that changes the appearance of the chest, while bottom surgery refers to surgery that alters the genital area.

Depo-Testosterone. Social and medical interventions like hormone therapy are often the first steps in gender-affirming care. (Photo: twitter.com)
Trans kids at a disadvantage
The mother of a 17-year-old transgender adolescent, who prefers not to be identified, says unless you live in Cape Town and are lucky enough to be accepted through the Red Cross War Memorial Hospital or Groote Schuur Hospital programme the only way to receive healthcare support is in the private sector.
“It is very expensive. Discovery Health has a pilot programme to support and affirm trans members but it remains limited and the barriers to entry are financially excessive with a lifetime limit of R200,000 in partial payment benefits,” she says.
She says there is no surgery for trans children in the public health system other than a few cases through Red Cross Children’s Hospital and before that is done, parental consent is needed.
Other surgeries tend to only be available to trans people from the age of 18.
“Young trans people do not always want or need surgery. The other social and medical interventions like hormone therapy are the first steps. What is often the case is that trans boys may need top surgery as soon as possible and this is the sort of initial surgery that a trans young person may need to remain alive. In South Africa, the only way for a minor to access top surgery will be through parental consent and in most cases at enormous cost in the private sector and then only with a surgeon who is happy to do this surgery,” she says.
She says less invasive surgeries such as top surgery are available through the private sector at an enormous cost. “Our son had top surgery at 14. All other surgeries remain an option for trans people and this is a very personal choice. We are researching surgeons in Serbia, Thailand, and the USA,” she says.
According to Pickstone-Taylor, the waiting list for surgery in the public health sector is so long that none of those under 18 would be still under 18 when offered surgery.
“Parents have to pay privately for top surgery and we work as a multi-disciplinary team to support those that want surgery before 18 and have parents who [can] pay for it. We have to ensure that the young person is psychologically prepared and supported enough to cope with surgery. Very few transgender male youth are lucky enough to have parents who can afford to pay for top surgery before 18 years old,” says Pickstone-Taylor, adding that their parents are always needed at this assessment.
The mother quoted earlier suggests that many transgender kids and teens are suffering from mental health problems in part because of the limited access to gender-affirming treatment. “This is why over 50% of transgender children try to kill themselves. The argument we made to Discovery Health to include adolescents in their pilot programme (it was previously only for adults) included all the clinical reasons but on a straight financial basis it is cheaper to affirm our kids than to have them in psych clinics trying to kill themselves every year,” she says.
Discovery Health had not responded by the time of publication.
But according to the Acting General Manager of Stakeholder Relations at the Council for Medical Schemes (CMS), Mmatsie Mpshane, the council has engaged the Department of Surgery at the University of Cape Town to discuss funding of gender reassignment surgery by medical schemes.
“It was established that the surgery was not [a] predominant and prevailing level of care across the South African public health sector. This implies that it is not Prescribed Minimum Benefit (PMB) level of care and funding thereof is subject to scheme rules, varying across schemes and dependent on [a] member’s benefit option or plan type. The CMS does encourage schemes to consider funding of these procedures as part of its yearly rule registration and approval process,” Mpshane tells Spotlight, explaining the PMB review process is ongoing with stakeholders’ inputs and participation. She said submissions relating to improved access to healthcare for all South Africans, especially vulnerable groups, are welcome.
Why access to gender-affirming care matters
Pickstone-Taylor says that 50% of transgender children will try to kill themselves if they do not get appropriate support.
“Children need social transitions,” he says, “for example when they request to change one or more of the following: name and pronouns, toilet change, and sports and school uniform change. If supported and allowed to socially transition, co-existing psycho-pathology invariably disappears the same day for pre-adolescent children. Equally, for adolescent children, suicidality and co-existing psycho-pathology disappear rapidly when allowed to take hormones to either stop puberty or cross-sex hormones. They are lifesaving in many cases,” says Pickstone-Taylor.
Chris McLachlan, the chairperson of the Professional Association for Transgender Health South Africa (PathSA), an interdisciplinary health professional organisation, says studies indicate that trans and gender diverse (TGD) people that are not able to access gender-affirming care have a 42% to 45% suicidality rate, meaning they would have attempted suicide in their lifetime.
“This [number] comes significantly down once the TGD person was able to access gender-affirming healthcare. Often, TGD people experience minority stress. Minority stress, he explains, is the stress that TGD people experience as they navigate a hetero-cisnormative world where they are marginalised, discriminated against, not accepted and affirmed, and even become victims of violence. We find that more TGD people suffer from anxiety and depression and this is often due to, or compounded by, the minority stress,” says McLachlan.

(Photo by Gallo Images/Darren Stewart)
Gender dysphoria
Clinical psychologist, Jordan du Toit says to be trans is associated with a condition called gender dysphoria, and while this is not a mental illness, it relates to the distress a trans person feels when their body does not match their internal sense of their gender.
“Gender dysphoria is associated with increased anxiety around your body and how it is seen by others, distress that your body does not match outwardly how you feel internally, and decreased pleasure in your body for things like sex, exercise, and daily living,” says du Toit.
This, du Toit says is a very traumatic experience to go through, and similar to other invalidating experiences (like sexism, racism, ableism) transphobia can be a real threat to trans individuals’ sense of acceptance and physical safety in the world.
“This can mean trans individuals mask or hide who they are to exist safely in the world or suffer from higher than average anxiety levels related to harassment and transphobia from others. The trans community is more at risk of suffering from post-traumatic stress disorder as a result of transphobic attacks, and this has a knock-on effect as it can lead to depression. The LGBTIQAP+ community at large is more at risk for suicide because of abuse and related depression,” says du Toit.
She adds that to be trans can be expensive.
“For a cisgender person (someone whose gender identity matches their biological assigned sex at birth), their bodies produce the hormones needed to maintain a congruent outward appearance. For someone who is trans, they need additional support for things like hormone therapy and affirmative surgery to help diminish gender dysphoria,” says du Toit, adding that the struggle to find affordable medical care can increase gender dysphoria and heightens the risk for mental illnesses such as depression.
McLachlan says the mental health risk is higher predominantly due to living in a world that is often unaccepting and also having to navigate a world that is not structured for diversity in gender and diverse gender expression.
“The TGD person needs to navigate an unwelcoming world, needs to navigate so many barriers and gatekeeping in various healthcare structures in order to live freely as the person they are and has to deal with rejection, hate, and marginalisation,” says McLachlan.
Trans persons at higher risk for HIV
A meta-analysis published in The Lancet suggests that internationally transgender women are as much as 49 times more likely to contract HIV than adults of reproductive age in general. Since the rate of HIV in adults of reproductive age in South Africa is extremely high, the ratio will be lower here — although that obviously doesn’t preclude the likelihood that South Africa may have some of the world’s highest rates of HIV infection in transgender people.
According to Nelson Dlamini, spokesperson for the South African National Aids Council (Sanac), HIV risk in transgender women is embedded in multiple co-occurring public health problems.
Speaking to Spotlight, Dlamini says there are high rates of unprotected anal sex among transgender women, which carries a higher risk of HIV transmission than vaginal sex.
“Several factors contribute to this stigma and discrimination, leading to low self-esteem and disempowerment [which] can make it harder for transgender people to insist on condom use. In many settings, condom use is often controlled by the insertive sexual partner, so many transgender women who have sex with men can feel unable to instigate condom use,” he says.
Dlamini further states that “gender-changing hormones, which some transgender women use, can lead to erectile dysfunction, increasing the likelihood of taking the receptive role during sex,” he says, adding that there are other social factors that make transgender people more likely to engage in high-risk sex.
Dlamini says studies have shown that some transgender people who want to affirm their gender identity through sex, or who fear rejection from sexual partners can be more likely to agree to unprotected sex.
“Evidence-based multilevel interventions that address the structural, biomedical, and behavioural risks for HIV among transgender populations, including transgender men, are needed to address disparities in HIV prevalence. Tailoring HIV testing activities to overcome the unique barriers faced by transgender women and men have increased rates of testing among these populations,” he says.
Towards solutions: Improving health systems
According to Gender Dynamix’s Adriana Beukes, there is a need for resources and sensitising of healthcare providers and administrators.
“There is a dire need for more trained and specialised doctors who can perform vaginoplasty, clitoroplasty and labiaplasty for women, and hysterectomy and oophorectomy, as well as metoidioplasty or phalloplasty, scrotoplasty/testicular implants for men,” says Beukes.
Beukes says part of the challenge is a lack of scientifically-based policy and protocols in the public health system which means that gender-affirming care is frequently seen as elective and non-essential, and is often only available at tertiary facilities if there is an endocrinologist who has a particular interest in providing the service.
“This,” she says, “leads to inequitable access to services. We need a state policy that recognises gender-affirming healthcare as an essential service and allows for the initiation of HRT (hormone replacement therapy) at other levels of healthcare facilities such as regional and district hospitals, and routine monitoring (including taking blood samples) and dispensing of medication at primary health care level,” says Beukes.
“We also need a standardised policy framework, with a national policy on the provision of gender-affirming health care, and for both state and private bodies and institutions to adopt the national gender-affirming guidelines (which are currently being drafted). The Council for Medical Schemes (CMS) needs to include gender-affirming health care as a prescribed minimum benefit so that it will be covered by medical aids, and when National Health Insurance is introduced, it needs to include gender-affirming health care,” says Beukes.
Department of Health responds
Spokesperson for the National Department of Health, Foster Mohale notes that several structural factors influence the vulnerability of transgender people and this is underscored by social marginalisation, stigma, and discrimination on all levels.
He says that the department recognises that gender reassignment surgery is a vital component of the transition process — from male to female and vice versa. “This is, however, a complex and multi-faceted process that not only includes genital reconstruction surgery but also may include facial feminisation, breast augmentation, and the use of hormones to enhance the body. This is a long-term process and requires medical staff with specialised knowledge and skills to support the path and to ensure optimal results,” he says.
Mohale says transgender people are one of the key populations that the department recognises as at increased risk of HIV acquisition and onward transmission. He says there are clear references to services for transgender people in the National Strategic Plan for HIV, STIs, and TB of 2017-2022, and in the Lesbian, Gay, Bisexual, Transgender, and Intersex (LGBTI) Strategy.
He says the National Department of Health is currently revising its High Transmission Area programme which has been renamed the Key Populations programme and this is accompanied by a Key Populations Health Implementation Plan as well as plans to establish Key Populations Centres of Excellence.
“The Centres will be established in public health facilities to ensure sensitive and relevant services for all key populations, including transgender people. We have developed a comprehensive Key Populations Competency and Sensitisation Toolkit and it is being rolled out to as many public health facilities, regional training centres, and to many health workers as possible,” he says. DM/MC
*This article was produced by Spotlight – health journalism in the public interest.



















 Become an Insider
Become an Insider
Comments - Please login in order to comment.