SPOTLIGHT
Second Covid-19 wave was ‘like a tsunami’ – Tygerberg doctor

Spotlight first interviewed physician and infectious diseases specialist Dr Arifa Parker in May last year as South Africa’s first wave of Covid-19 was building up. Eleven very difficult months later, Spotlight checks in with Parker to hear how things are going on the frontlines at Tygerberg Hospital.
On December 15, physician and infectious diseases specialist Dr Arifa Parker spent her 40th birthday on call at Cape Town’s Tygerberg Hospital.
Her four-year-old twins Yusra and Haniya were being looked after by her mother.
On that day, 7,552 people tested positive for the novel coronavirus around the country.

A Covid response team meets at Tygerberg Hospital. (Photo: Nasief Manie / Spotlight)
Six days earlier, Health Minister Dr Zweli Mkhize had announced South Africa’s Covid-19 “second wave”.
Parker is in favour of tightening restrictions this Easter weekend – including introducing an alcohol ban – to reduce trauma admissions to hospitals and avoid the kind of social mixing that could trigger a third wave.
‘Totally overwhelmed’
“The second wave was like a tsunami,” she recalls. “I remember clearly when it started… It was the 13th of November, a Friday. We just had this steep rise of Covid admissions and within a week, our high care wards were full.
“If I have to be honest, in the initial weeks we were totally overwhelmed. At Tygerberg, we were at least blessed with an absolutely amazing team.”
Since January 2020, Parker, one of three infectious diseases specialists at Tygerberg, has served in the frontline of South Africa’s fight against Covid-19. (Spotlight previously interviewed her in May 2020.)
Along with other healthcare professionals countrywide, Parker had to allocate limited resources to patients and make those who were dying as comfortable as possible, all the while gathering information and formulating protocols for how to best tackle this new pandemic. It was akin to assembling an aircraft in mid-air.
As if that’s not enough, Parker is also working on a PhD on the links between HIV, obesity and SARS-CoV-2.
“If there’s one thing we should emphasise, it’s that Covid is also an infectious disease of lifestyle,” she says. “It’s a wake-up call for us to start living healthily… to start exercising.
“Severe Covid is due to uncontrolled inflammation triggered by the virus. Through exercise, you can increase a key enzyme which can counteract this inflammation.
“My recommendation is for people to get out there, exercise, start running, eat healthily – because the majority of the patients who die from Covid or land up in critical care appear to be overweight.”Parker is speaking to Spotlight through her face mask inside Tygerberg’s buzzing cafeteria. Around us, people have removed their masks to eat. “Keep your mask on,” she says. “It’s safer.”
She scrolls through her phone to find a photograph circulated on their staff WhatsApp group. It shows Parker sitting against a wall, staring at her phone. “Happy birthday, Arifa. It is what it is,” reads the caption. “I’m in an office next to a high care ward,” she says, laughing. “It was a staff meeting on my birthday.”
‘Overwhelming volume of admissions’
The doctor, eyes shining above her mask, laughs often. Perhaps it helps dispel the discomfort always at the periphery of her job. Death is no easy subject. But, she says, while the second wave death rate had been overwhelming, she prefers to focus on the recoveries.
“It was bad in the second wave… brutal,” she says.
“A lot of patients died, largely due to the overwhelming volume of admissions. Percentage-wise, the death rate was higher in the second wave, probably not because of the different variants, but because hospital systems were overwhelmed by the sheer number of patients.
“At Tygerberg, the survival rate for the first and second waves was about 70 to 75%. If you are on high-flow oxygen, survival is approximately 50 to 60%. Once you are intubated, the prognosis is really poor. Not just at Tygerberg, but across the province. Even in private hospitals and internationally.”
She adds: “I have to admit the second wave floored me. While I was covering high care, I would see, for example, that this could be me: this could be my best friend, this could be my husband.
“For me, the hardest was a 27-year-old male who came in, and, you know, we’d done everything we could.” He died after developing myocarditis, a weakening of the heart muscle, due to Covid-19.
Was the patient profile different in the second wave?
“I contacted the NICD (National Institute For Communicable Diseases) to discuss this,” says Parker. “The NICD put together a document that compared patients in the first wave to the second wave. And, actually, it’s not different. It was just that the volume of patients was so high that we would see more younger patients, too.”
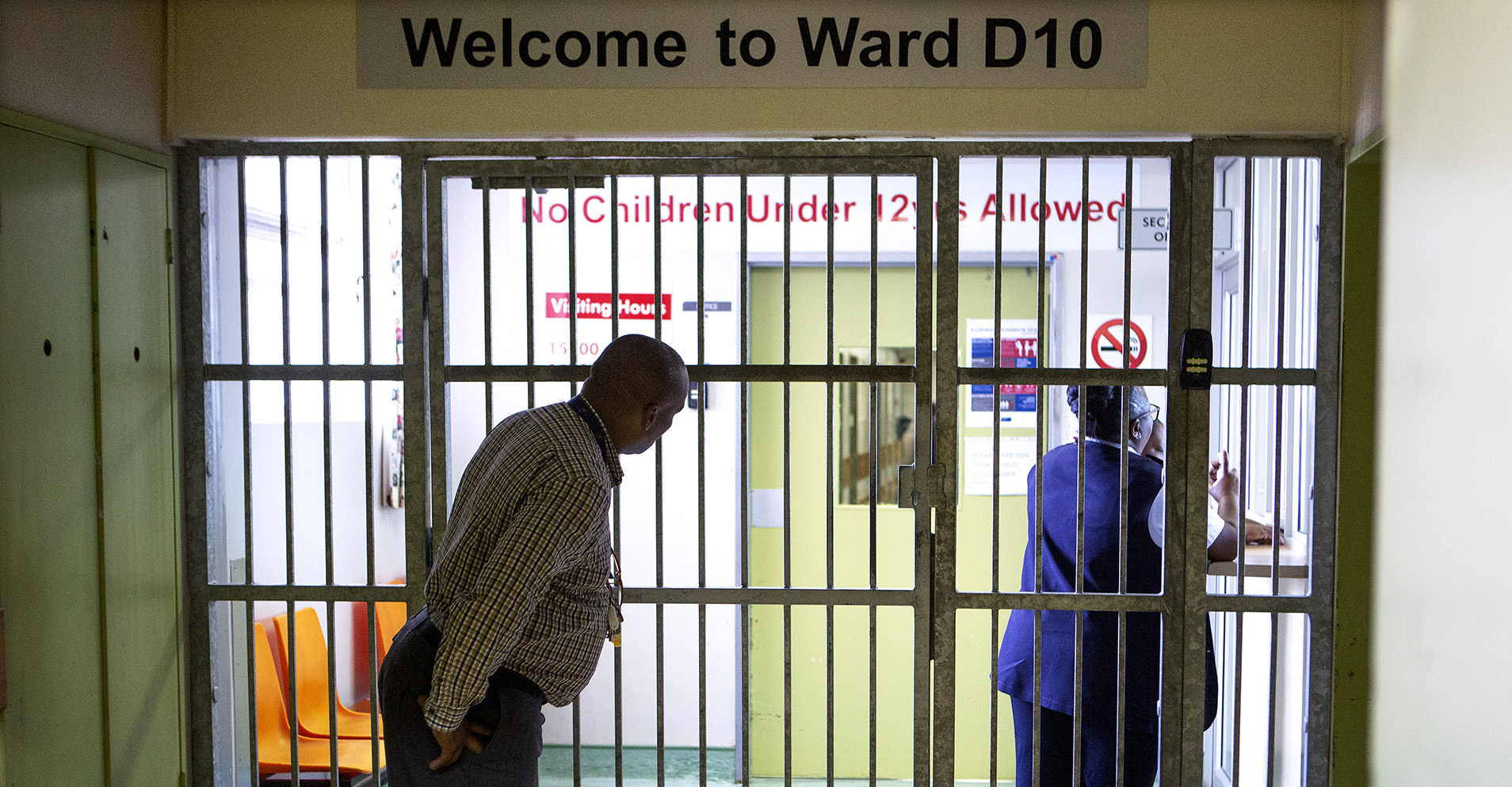
Ward D10 isolation unit during a media briefing to discuss the first case of Covid-19 at Tygerberg Hospital in Cape Town on 11 March 2020. (Photo: Gallo Images / Misha Jordaan)
Having to decide which patients would receive life-saving resources over others was heartbreaking, even though such decisions were informed by the Western Cape health department’s critical care triage tool. The tool scores patients based on their prognosis, so resources can be used to help people with the best chance of survival.
“In a resource-poor setting, what they use is age, the presence of comorbidities, illness severity and so on, to see whether ICU care would make a difference or not. For example, if you only have one ventilator… from an ethical or triage scoring point of view, the ventilator would go to the patient who would benefit from it the most. It’s very difficult.”
Another hard lesson learned from the second wave was the importance of palliative care.
“If you know that a patient’s prognosis is very, very poor, it might be kinder to offer palliative care earlier, as opposed to, you know, us doctors pushing and trying our best,” she says.
“So a lot of these difficult issues came out. Some doctors are so reluctant to pass their patients over to palliative care, because they see it as failure, when it is actually providing the best to our patients in terms of dignity in their last days,” Parker says.
“At Tygerberg, our oncology department ended up stepping in to help with palliative care. The nice thing about working at Tygerberg is that from the start we approached this as a whole hospital response, as a team effort.
“Almost every department in the hospital had a part to play in the Covid response. We had ENT [ear, nose and throat] doctors assisting; dermatologists, who just normally look at skin, managing pneumonia; ophthalmologists, surgeons, plastic surgeons. All of these departments, led by the department of medicine, helped manage our patients. We just had to work together to get through it.”
At the same time, there were many other patients needing treatment for non-Covid-related ailments. Parker sighs.

A sign at Tygerberg Hospital in Cape Town, on Sunday, 29 March 2020. South Africa went into a nationwide lockdown for 21 days in an effort to mitigate the spread of Covid-19. (Photo: Gallo Images / Nardus Engelbrecht)
“So this is very, very hard again. The Covid wave was so overwhelming. As an example, our normal medicine admission rate would be approximately 20 to 40 patients a day. And for the weeks of peak Covid, we were admitting 70 patients a day. So you have double the patient load with the same number of staff.
“You know, staff are not going to fall out of the sky… we don’t have the luxury of creating new staff overnight. So something had to give. Thus we were forced to de-escalate certain services in order to escalate Covid services. That had to be done. There was no other way to do this.
“Like I said, if a patient is admitted with Covid, they are more likely to live than die, as it is a treatable illness,” says Parker.
“I mean, if you don’t give oxygen to a patient who needs it, they will die. So after the first Covid wave, we saw a lot of neglected TB cases and other illnesses. There are a lot of ethical issues that came into play.”
‘Staff, stuff and space’
Parker draws two graphs in a notebook, illustrating “pandemic response”.
“There are ways to manage a pandemic. You can flatten your curve. So maybe if we had the alcohol ban earlier in December, there would have been less mixing and our curve would have been flatter. Simultaneously, we need to raise the healthcare line… for this we need three things: staff, stuff and space,” she explains.
“Our big problem is staff. The stuff, we have – we have enough PPE, ventilators and so on, thanks to donations from organisations like Gift of the Givers. Wow, I cannot explain how grateful we are to that organisation. Space, we have – we can create more wards. But staff…”

Tygerberg Hospital. (Photo: Nasief Manie / Spotlight)
Parker says it would be naïve to think a third wave will not happen.
“We are already preparing our third wave response. We would rather over-prepare, like we did for the first wave, than be fairly under-prepared, like we were for the second wave.”
‘Our only hope’
After she touches any surface, Parker sanitises her hands.
Looking around, she says mealtime is a risk. “I worry about mixing when there is food in a closed space. Now your mask automatically goes off, and you are talking, laughing, with lots of little droplets spreading.”
She leads us through the hospital, past a sign reading “vaccinations on the fifth floor”. She shakes her head, saying that vaccine allocation remains controversial. Parker was vaccinated three weeks ago.
“The few vaccinations we’ve done in South Africa are not going to make a difference to the third wave,” she says. “But it’s our only hope at this moment, and I think it’s the safer option as opposed to having everyone wait for natural immunity.”
We pass the hospital’s dispensary. It’s packed with people sitting in chairs with an empty seat between each other. Inside an elevator, she presses the button with her knuckle. “This is how you do it to be safer,” she says.
On the eleventh floor, the hospital’s Covid-19 response team is gathered for their weekly meeting. DM/MC
This article was produced by Spotlight – health journalism in the public interest.
"Information pertaining to Covid-19, vaccines, how to control the spread of the virus and potential treatments is ever-changing. Under the South African Disaster Management Act Regulation 11(5)(c) it is prohibited to publish information through any medium with the intention to deceive people on government measures to address COVID-19. We are therefore disabling the comment section on this article in order to protect both the commenting member and ourselves from potential liability. Should you have additional information that you think we should know, please email [email protected]"





 Become an Insider
Become an Insider