Does this mean a second wave is inevitable in South Africa?
In South Africa, the possibility of such a resurgence has seemingly justified the extension of the powers of the National Covid-19 Command Council (NCCC), under the legal framework of the National Disaster Management Act.
While this appears consistent with the country’s strategy, it is unwise to simply extrapolate outcomes from the current resurgences in Europe and apply them to South Africa, more so given the extra-parliamentary posture of the NCCC and concern over the lack of transparency in its decision-making process.
This abundance of caution is critical to avoid reflexive interventions for the ongoing management of the pandemic, especially in anticipation of a resurgence (or “second wave”) such as that being experienced in Europe and elsewhere.
It is imperative that knowledge of transmission and exposure patterns relating to SARS-CoV-2 in SA’s own setting must inform a calibrated and transparent response, not least because the most important component of the response is willing and voluntary compliance with mitigation measures by the public.
What is the rationale for European countries to impose lockdown strategies to manage the resurgence?
The United Kingdom, France, Netherlands and Spain have introduced a new round of curfews and are considering lockdowns as a means to contain transmission. Such interventions might well be effective in these and other countries, especially if they are able to support a lockdown from a societal and economic perspective.
These measures are also underpinned by the low levels of immunity in the general population in the affected regions. The majority of EU member states still have low levels of seropositivity (see Germany here and Spain here) to antibodies directed to SARS-CoV2, ranging between 0.9%- 8.5%. Regions in some countries are outliers such as Austria, with more than 40% seroprevalence of Covid-19 antibodies detected in its populace due to heavy infection in the first wave.
These data suggest that in certain European countries, such stringent measures may retard transmission and therefore the overall number of cases and deaths.
Should the same rationale apply in South Africa?
We believe the context is different in South Africa.
Countries implement public health measures to get transmission under control. To get transmission under control, countries have two choices.
First, they can try to reduce transmission in order to reduce a peak health demand. This is called mitigation. Mitigation can be achieved by isolating cases and quarantining close contacts (requiring a robust test and trace capability), adherence to social or physical distancing, wearing masks, hand hygiene and protecting that part of the population with the highest risk of serious illness if they are infected. Collectively, these measures are termed non-pharmaceutical interventions, or NPIs.
Second, a country might attempt to suppress the epidemic and attempt to stop transmission. This is called suppression or lockdown and aims to reverse epidemic growth, reducing case numbers to low levels by physically distancing the entire population indefinitely.
Seven months into the pandemic, it is evident that while SA’s hard lockdown at an early stage of the epidemic initially slowed transmission, and that some healthcare facilities in certain areas of the country were able to prepare for the expected increase in admissions, this was uneven and did not manage to stop transmission. There is even less chance now of being able achieve sustained suppression of virus circulation in South Africa through a lockdown, than was the case when circulation initially started.
South Africa, despite having one of the earliest and harshest lockdowns for a protracted period of time did not achieve suppression, nor was it likely to.
The reasons for this are self-evident:
- The lack of an integrated approach to the SARS-CoV-2 outbreak, from initiating community screening and tracking Covid-19 disease outcomes;
- The inability to scale-up community testing in time, with concomitant long turnaround times and inadequate contact tracing that would enable the timely isolation of cases and close contacts. Contact tracing was not achieved at the scale required to suppress the epidemic, despite SA having one of the largest testing programmes in Africa.
- Compliance with lockdown rules and NPIs suffered a trust deficit arising mainly from poor communication, heavy-handed enforcement and random bouts of misinformation from dubiously qualified private lobbies.
The international experience is illuminating.
Except for a few island nations, most countries failed to achieve sufficient viral control, whatever mitigation or suppression measures were applied. The World Health Organisation (WHO) actually concurred with the view of some local scientists who had cautioned against a hard lockdown as a primary strategy prior to its imposition.
It was clear that a lockdown alone will not eliminate or permanently control the spread of the virus unless it was coupled with an efficient system of testing suspected cases of Covid-19 and ensuring their isolation, as well as exercising a high level of contact tracing and their proper quarantine.
The reality is that the massive societal, economic and health resources needed to emulate countries like South Korea and China, which were initially able to achieve impressive levels of suppression, were not available to countries like SA. Moreover, while the rate of virus infection can be controlled through measures such as NPIs, adherence to even these measures are challenging in most low income settings where overcrowding is a grim reality, and even access to water is compromised.
Consequently, the highly restrictive and even coercive lockdown measures deepened social discontent the longer the measures were in place; the enforcement of which deepened mistrust of the authorities and may have contributed to poor compliance with mitigation measures in all groups and classes of society.
Alongside an inadequate testing and tracking infrastructure, this resulted in only a temporary reduction in community transmission of the virus over the first three to four weeks of the lockdown.
However, failure of being able to test for Covid-19 at scale in the public and private sectors, plus the incoherent prioritisation in the testing regime and the delay in turnaround times of tests, as well as the incapacity related to the tracing of contacts and their quarantine, have led to the predictable consequence that community transmission persists and may yet seed another increase in cases.
Reproductive Rate of the South African epidemic under various stages of lockdown
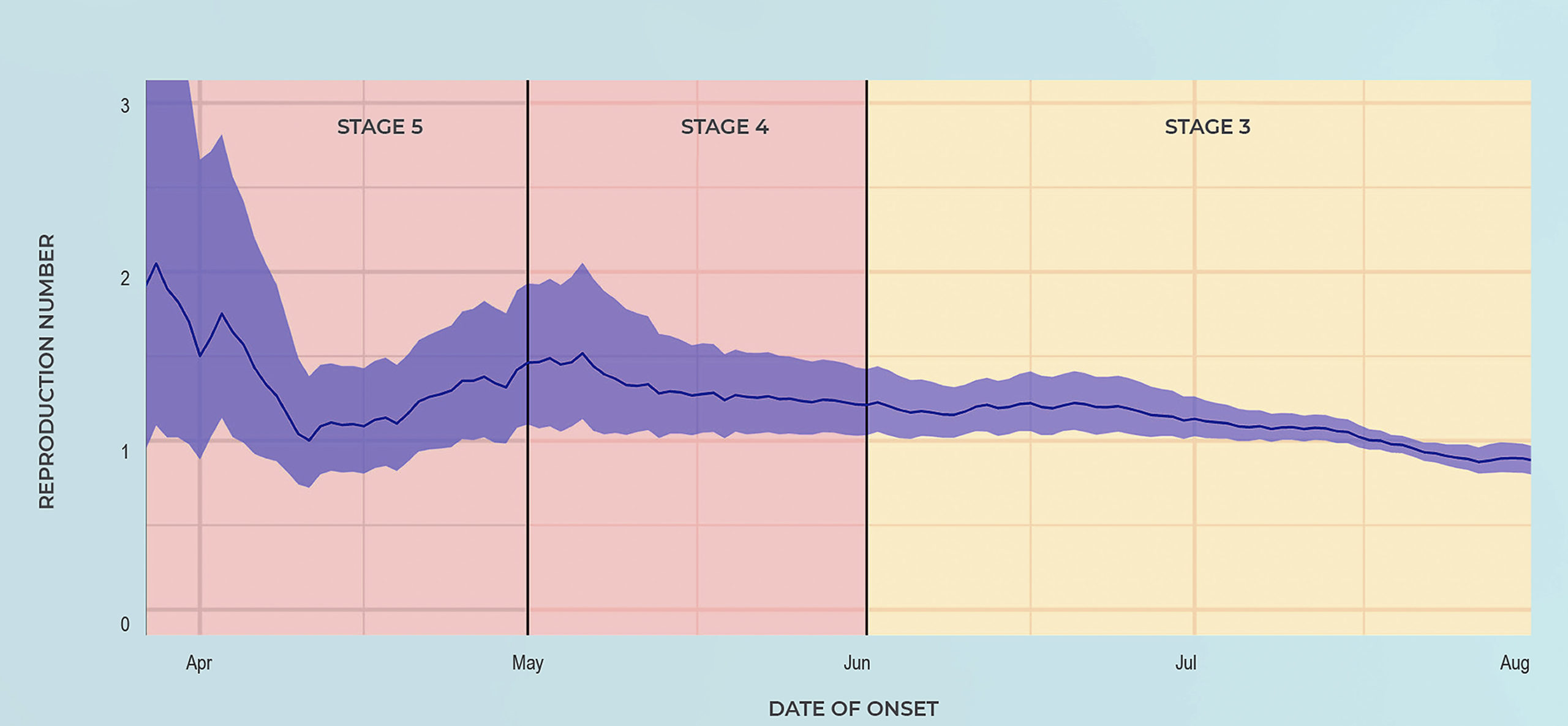
Source: National Institute of Communicable Diseases.
This persistence of transmission is evident through an analysis of the effective reproduction rate (Re) of SARS-CoV-2 as modelled by the National Institute for Communicable Diseases (NICD). The effective reproductive rate determines whether the number of cases of Covid-19 in the population will go up (when Re >1) or down (Re <1).
In South Africa, during the Level 5 lockdown, the Re ranged from around 1.5 to 2, indicating ongoing community transmission even during the lockdown.
The Re only declined substantially after the surge in July, following large scale exposure to the coronavirus in various communities in the Western Cape and Gauteng, thereby reducing the number of people susceptible to infection.
At the time of lockdown Level 3, up to 40% of the population in the Western Cape (and empirically a similar percentage in major urban metro areas in Gauteng) demonstrated evidence of SARS-CoV-2 infection, including presence of antibodies to Covid-19.
Seroprevalence surveys in Western Cape
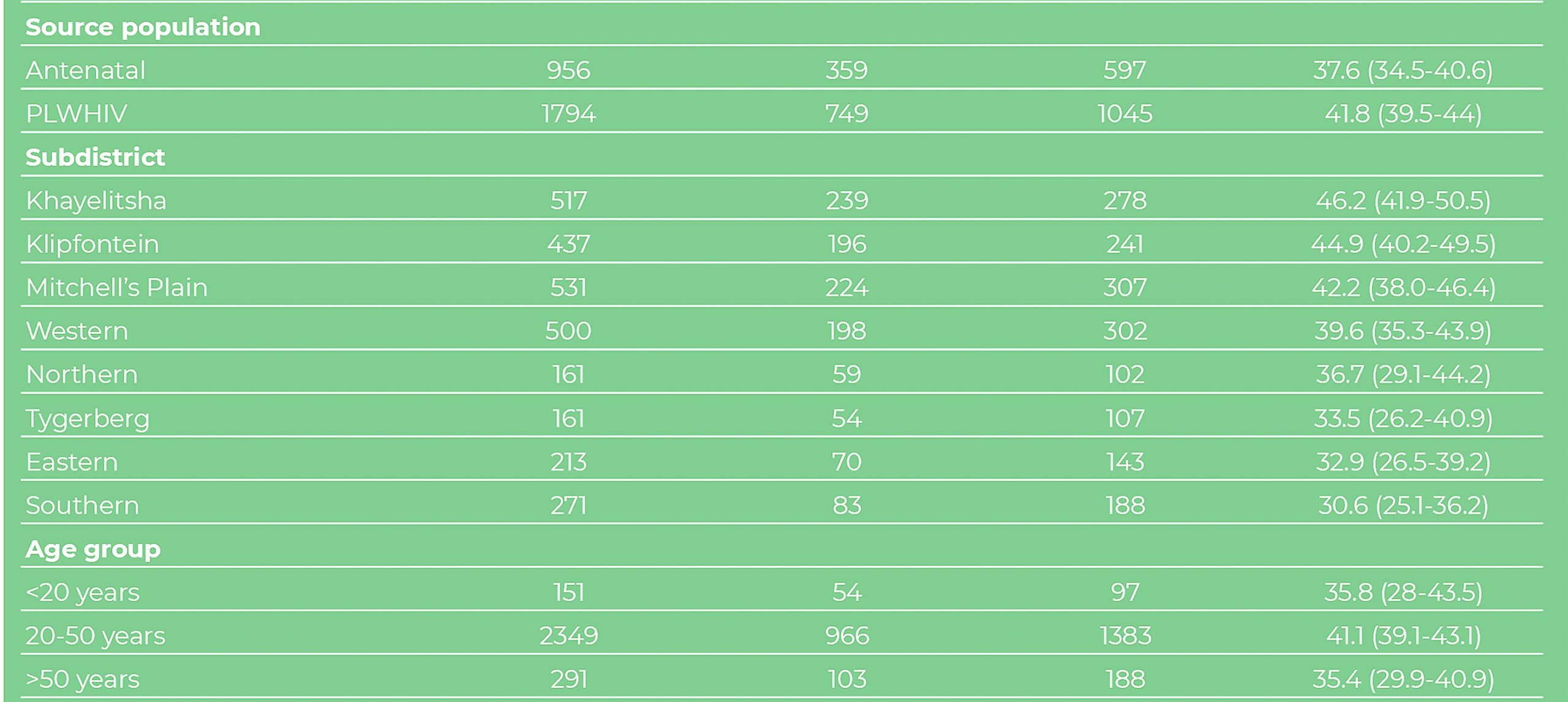
Source: National Institute of Communicable Diseases.
Did lockdown or mass exposure to SARS-CoV-2 lead to subsidence of the first wave?
Data suggest any claim that the highly restrictive lockdown was successful in preventing community transmission of the virus, and contributed to the first wave waning, is inaccurate. Paradoxically, infection rates only started declining and the Re trended downward to approximately 1 from July onwards, as restrictions were being eased and social and economic activity increased commensurately.
The proposition that the interruption in the chain of transmission of the virus – due to an increasing proportion of the population being gradually infected over time and developing at least partial immunity – is supported by surveys undertaken across different districts in the Western Cape, where 40% of women attending antenatal clinics, and people living with HIV, had evidence of infection in different sub-districts, suggesting that a massive “covert” wave of infection, far greater than in Europe, North America or Asia (excluding South Asia), occurred.
Certain practices such as maximum taxi occupancy and resumption of attendance at places of worship, which were incrementally allowed during relaxation of the lockdown, undoubtedly increased the risk of virus transmission to people still susceptible to infection.
Despite some reluctance to comply due to inadequate communication coupled with harsh enforcement, the partial adherence to NPIs may have somewhat mitigated the potential consequences of these actions and was the most effective aspect of our public health interventions.
Notably, the recommendation by the previous ministerial advisory committee for the use of non-surgical face masks – and emphasising the potential airborne transmission of SARS-CoV-2 in South Africa – preceded WHO recommendations and advisories on these measures.
Paradoxically, the approach to lessening lockdown restrictions as the epidemic gained momentum in South Africa, likely led to a massive surge in coronavirus infections during our winter months, inducing at least some immunity in a high percentage of the population, particularly in densely populated areas.
This most likely led to an interruption in the chain of transmission of the virus in South Africa, which, together with at least partial adherence to NPIs, resulted in the first wave of the epidemic waning.
However, the proportion of the population that has been infected is likely far less than what is estimated (60-70%) to enable sustainability of low rates of infection (Rt<1.) – so called “herd immunity”.
There is also evidence of increasing complacency around the adoption of NPIs.
Therefore a resurgence of Covid-19, consequent to declining adherence, is likely to be experienced in the short term. Furthermore, uncertainty regarding the longevity of immunity following infection makes projections difficult on the future course of the pandemic.
What can we learn from other countries and does it predict what will happen in South Africa?
One observable similarity between South Africa’s and Europe’s epidemics has been a reduction in cases correlated with a change to warmer seasons. Although climatic factors may play some role in the transmission of SARS-CoV-2, the role of changing human behaviour in reaction to the weather is probably the deciding factor.
Spending more time outdoors and the ability to ventilate closed (taxis, trains etc) and indoor spaces is a critical factor.
One lesson, however, is important: the opening up of European societies during the summer months was likely coupled with less adherence to NPIs, which allowed for a resurgence of infections and Covid-19 hospitalisations.
In South Africa, our adherence to these tried and tested public health interventions to control Covid-19 must continue unabated. This is absolutely critical if we are to be spared the worst ravages of the kind of resurgence being witnessed in the northern hemisphere.
Different testing rates and testing strategies in many of the European countries (including Spain and UK), make it impossible for head-to-head comparison of the scale of the resurgence, relative to what was experienced in their first waves. Similarly, we cannot make meaningful head-to-head comparisons between (and even within) countries in respect of the number of infections or death rates that may result here.
This makes the task of gaining any insights into what could happen in South Africa inordinately difficult. After all, the hard lockdown initiated in SA followed the examples of China, South Korea, Iran and Italy, all of which experienced high-surge phenomena, even before the virus took hold in the South.
As we have noted above, this was perhaps not the optimal response, given what we already knew about local epidemiological trends and the extreme unlikelihood of countries in Africa being successful when aspiring for containment of a respiratory virus.
Resurgence is likely but our response should be different
A resurgence of Covid-19 is certain to occur in South Africa, although indications are that a second wave is likely to be different to the wave currently sweeping over Europe.
It is possible that, because a large percentage of people who live in major urban metros with a high population density have already been infected, this will assist in limiting the rate of transmission in such settings.
Put another way, a resurgence in settings where there was a high force of infection during the first wave, is likely to be of a lower magnitude than experienced with the first wave. Conversely, communities with low rates of infection in the first wave, may be disproportionately affected during a resurgence of Covid-19.
Seroprevalence surveys designed to characterise the proportion of communities that have been infected during the first wave in all sub-districts of South Africa will be a vital indicator of where a resurgence of infection might be concentrated.
Provinces and communities which experienced a lower rate of infection in the first wave may be settings for higher rates of infection and mortality in a second wave if mitigation measures are not implemented.
Strategies to meet this expectation, including smart, targeted and strictly limited restrictions, must be urgently devised and based on credible and swift seroprevalence surveys and a rational and outcome-driven testing programme.
Active adherence to public health measures and building robust test and trace infrastructure, as well as strengthening healthcare infrastructure in anticipation of an increase in cases, are likely to be the deciding factors in how well the country navigates resurgence of Covid-19.
What we can be certain of is that the type of hard lockdown imposed in March will only inflict further, perhaps fatal, damage to an economy which was on the ropes before the pandemic – and which the hard lockdown rendered moribund.
It will also significantly undermine any chance of an economic recovery, without achieving any meaningful net health impact.
It is, moreover, unlikely that a Covid-19 vaccine will be available to South Africa before the end of the next winter. Consequently, the only instruments in our current toolkit to blunt and minimise the consequences of a resurgence is to actively motivate society to continue adhering to NPIs.
Even if NPIs are not always implementable at scale in our own context, they nevertheless contribute massively to the control of the rate of transmission of the coronavirus and would assist in avoiding overwhelming the beleaguered healthcare delivery system.
It is axiomatic that only the people can overcome a pandemic, as observed throughout history.
It is, therefore, the work of governments to act in support of – and not second guess – the scientific and health system imperatives.
To single-mindedly focus on providing the people with all the necessary information and support, and to eschew self-serving political considerations in this effort, represents the most important contribution of South Africa’s political leadership in this time of crisis. DM/MC
Professor Shabir Madhi, Respiratory and Meningeal Pathogens Research Unit, University of the Witwatersrand; Professor Glenda Gray, South African Medical Research Council; Professor Francois Venter, Ezintsha, University of the Witwatersrand; Professor Marc Mendelson, University of Cape Town; Dr Lucille Blumberg, National Institutes of Communicable Diseases; Dr Aslam Dasoo, Convener of Progressive Health Forum.






 Become an Insider
Become an Insider
A brilliant article – thank you. For the first time I’ve managed to get my head around the “how and why” questions about this virus…… this very constructive article should become the Bible for all medical professionals and the Covid Task teams. Trump should read this too as the virus in his rural States start to surge…..the bottom line is “ wear a bloody mask!”
I question the comment “the only instruments in our current toolkit to blunt and minimize the consequences of a resurgence is to actively motivate society to continue adhering to NPIs”. It is as if the role of elevating community levels of Vitamin D and Zinc and the use of Vitamin C have been completely discounted. A one liner from this Concerned and highly trained and experienced group of Scientists would be useful.
As @Jane Crankshaw said, a ‘brilliant article’. In my case it has also been the best article I have read explaining the transmission of the virus.
Regarding the wearing of masks, I work remotely on a project team with colleagues in the West USA and they are adamant they will not wear masks and that the virus is a scamdemic. Unbelievable, but they drink the Trump coolaid.
A somewhat lengthy but brilliant article for those who want to increase their understanding of the pandemic. Non-pharmaceutical interventions (NPI) do assist in reducing the spread of the virus; in short wear masks and keep your distance.
1. Let’s mention the effectiveness of vitimin D and zinc.
2. Society needs to be aware of hospital beds capacity.
3. Society needs to be aware of ICU capacity.
4. Society needs to be aware of addition deaths.
5. With this critical information any reasonable person can decide on their appetite for risk.
6. The difference in doing everything right in the suburbs where the infection percent was 30 while townships 40 percent in my opinion makes the lock down and every other activity a complete waste of time and money.
7. No mention is made of numerous medical doctors and nurses saying this was a pandemic but now it’s normal flu.
Telling a population to wear a mask all the time has turned it into what I call “the mask game”. Most people’s mask wearing practise is doing more harm than good. They continually touch their faces putting them on and off, they wear them when out walking when they should be breathing freely while exercising their lungs for maximum protecting from respiratory viruses, they dont wash them regularly, they even share them. For the miniscule benefit that they may have surely it would be better to tell the people to only wear when indoors and in a crowd where distancing more than a meter is not possible? This is what WHO recommends in any case.
Eventually we see a crack of professional lucidity shining through the thick clouds of alarmist guff. A few points: you mention credible and swift seroprevalence surveys. Why is the preferred method of detection the Polymerase Chain Reaction (PCR) test? For readers who are not familiar with it, the polymerase chain reaction is a method widely used to rapidly make millions to billions of copies of a specific DNA sample, allowing scientists to take a very small sample of DNA and amplify it to a large enough amount to study in detail (Wikipedia). The problem being, according to it’s inventor biologist Kary Mullins, it was developed for research and not diagnosis because when trying to detect a specific virus it can, and often does, give a false positive. Mullins explicitly said as much when it was wrongly used to diagnose HIV. Unfortunately Mr. Mullins died of pneumonia in September of last year, just prior to the infamy of Covid-19, or he would no doubt have said as much again. Then we have the definition of what is called a “case”. In medical terms a case is generally considered to be a person who is infected, presenting symptoms and therefore contagious and requiring medical treatment. An asymptomatic person is not considered a “case” because they are not infectious and require no medical care. In the response to Covid-19, any person found to be “positive” using the anyway inaccurate PCR method, is considered a “case” whether they present symptoms or not. It’s curious, to say the least, as to why the PCR test still being used. In conclusion, it has become painfully clear to the rest of the world that the tried and proven approach favoured by Sweden was the correct one. Isolate the genuine cases and protect health workers and the vulnerable. Any harm to society caused by a virus from which we have a better than 99.9% recovery rate is minuscule compared to the harm and mortality associated with the draconian response of lockdown. Besides P2 or N95 masks intended as for PPE for health workers, there is also very credible evidence to suggest that the wearing of masks for anyone not displaying symptoms is pointless.
If around 40% of WCape had antibodies in June, then that number by November must be much higher. We still don’t know how long immunity lasts, but we do know that those that were non-symptomatic first time around are extremely unlikely to have a worse time the next time. If our population has say 60% “immunity” then a massive second wave of patients (not infected, people that need hospitals) is very unlikely?
Jane I wonder if you have children? I can assure you that seeing my children going to school every day with a mask and being forced to keep them on all day even when doing sport and being outside for break time has distressed me beyond belief. There is no logical sense to this and the devastation physically and emotionally on all those millions of children out there being literally threatened with death if they remove their masks is criminal, actually child abuse. No I’m not a Trump supporter, just a concerned mother who has seen first hand the effects of this practise. Feeling helpless while knowing what we are doing is inherently wrong and unsustainable.
A forlorn hope I fear Jane Crankshaw. Even if Trump does read this article, there is little doubt that he’ll take it to heart.
Would be good to see more widespread sero-prevalence surveys done. I fear that too much stock is being placed on a fairly small and unrepresentative sample of a few thousand pregnant women and HIV+ve people that had blood taken at clinics and hospitals in the Western Cape.
Here’s a one liner on vitamins “there is no credible evidence that vitamin D, vitamin C or zinc have any role in the prevention or treatment of COVID-19”. Treatment protocols for ‘respected’ ICU doctors is NOT evidence. If you can find randomised controlled trial evidence for the benefit of any of these interventions I will happily look at it, and if the evidence is credible I will gladly endorse them. Tom Boyles Professor of Infectious Diseases.
If this, or other viruses, are likely to be with us forever are we always to be subject to NPI regulations? We lived with all other communicable diseases through good hygiene and medical support happily before March 26th. I respect the choice of anyone who wants to keep distanced from everyone and wants to wear a mask and not go to sporting events and other major entertainment events for fear of contamination but I am not scared and I want to go to these events and I want to build up my own immune system through contact with others, and sometimes I will get sick and sometimes I won’t. I guess if anything comes out of this article it has to be about knowledge gained from SA’s experience and the risk and reward of NPI’s. 700,000 known infections in 8 months out of a population of 58,000,000 ish is a low infection rate and with 18,000 deaths there is a low death rate from infection, which gets lower if, as the article suggests, infection rates are considerably higher than we think. The reward of NPI’s is a low perceived death rate but with dire consequences for the economy and society, the fallout from which we have not even begun to see yet as people become desperate for the basics in life. I am at a loss as to how this government can ever extract itself from the state we find ourselves in now regarding Level 1 and NPI’s (social distancing, endless sanitising, mask wearing and restricted social events) . Human beings are inherently social and this state of being will lead to inevitable breaking of these restriction. I believe we have enough information now to allow a removal of restrictions 100% in the country and if you want to sanitise all day, wear a mask and keep away from people that is your choice, me I choose not to if thats OK?
Good article.
But we need to be doing much bigger seroprevalence studies. We can’t be relying on one smallish study from Cape Town in July.
Our number one priority for 2021 must be to have a normal school year. It is terrible to see here in the rural areas how many learners are using the Covid disruptions as an opportunity to drop out of school entirely. We are seeing attendance rates of 20% in our rural schools and children getting only 2 days of classroom time per week.
In 2021: no platooning, normal class sizes, normal school hours and 5 full days of school per week.
It is quite evident from many responses that there are several (not all) people here (not just supporters of the Trump cult in the US) who for less outrageous reasons are opposed to the use of masks!
Why are there so many mask denialists?
The article above, written by 6 experts, supports mask wearing. Every legitimate study has shown that masks have an effective impact on spreading Covid. A recent study from University of Washington predicts that up to 130 000 American lives could be saved if 95% of the population wore masks. (https://www.medpagetoday.com/infectiousdisease/covid19/89302)
But still so many are opposed? This “it’s my life and I will live it as I want” is just so revoltingly shortsighted and selfish. Wearing a mask protects not only you, but people around you. Can you not bear the discomfort of a little piece of material in front of your faces to help others? I mean, seriously, is it really that hard?
There are mask denialists because the science supporting their use in the population at large is poor. The global narrative on mask use did an abrupt U turn in June for no apparent scientific region. A “gold standard” randomised controlled trial undertaken in Denmark by reputable investigators has been denied publication in a number of medical journals. Hopefully NOT because it contradicts the politically correct approach? Interestingly, the famously non mask wearing Swedes have not experienced an increase in deaths despite an increase in positive tests, unlike other mask wearing European countries. Perhaps it is time to accept this is yet another disease mankind must live with and get on with our lives without authoritarian regimes trampling on civil liberties. Sorry to disappoint all the COVID pessimists out there, this too shall pass, whatever we do. You can move on to worrying about the devastating health and economic effects of the lockdown.
Sorry Martyn, the stats don’t back you. Compare Sweden, Finland, Norway. A prettty homogenous grouping. Sweden had roughly ten times their neighbors death rate and three times the infection rate. For me, we have to get the antibody testing sorted out especially for frontline workers. There must be an enormous difference in risk management of your workers if you know which are 100 times safer than the others. So Mary can work at reception but rather have John work from home.
Hi Johan I appreciate what you are saying . Sweden made a mistake in not protecting their vulnerable early enough. They are different to their neighbors in terms of population density and of course there are many other variables. My point was the absence of an increase in deaths despite an increase in positive tests. Like Tom Boyles I prefer my medicine evidence based. RCTs are sadly lacking amidst the pandemic hysteria. Antibodies are only a part of the immunological equation, we will probably pondering this 30 years on , as we are with HIV. A vaccine may never happen. In the mean time, let’s try to work together to minimize the unfolding tragedy of the consequences of a fruitless lockdown. Leave managing the residue of our epidemic to health care professionals who are actively involved in clinical care. They have performed exceptionally. Exclude politicians, “scientists/modelers” and anyone who has a financial interest .
Where does this mask issue come from? I have a child and “schooling at home” was bad (for kid and parents), as was not seeing friends, doing sports, music, outings etc. Wearing a mask? He hardly notices. One of several sacrifices to make daily life safer and allow to regain some degree of normality. Small price, big gain. Most counterarguments are trivial and in light of the pandemic and its medical and other costs actually quite ridiculous… (I notice that most working class people seem to wear masks quite happily, while their clients whine. I am not a sociologist or psychologist but wonder about a luxury problem of the affluent with no existential needs or threats…)
I totally agree with the core arguments of the article: We will likely experience a second surge, that a new lockdown cause unsustainable economic damage, and that measures to reinforce adherence to NPI’s will be our best, if not only hope to keep infection rates under control for the foreseeable future.
However, much of the article meanders into the muddy waters of herd immunity thinking, with not a clear enough disclaimer from the authors that the underlying hypotheses have not yet been proved or disproved by scientific studies. It is possible that future history and scientific studies will prove correct the notion that a high percentage of people in the Western Cape and Gauteng have gained some degree of immunity due to exposure to the virus, and therefore Western Cape and Gauteng may be spared much a of a second surge. However, this is by no means a given.
Firstly, an assumption that the positivity rate of tests on women at antenatal clinics is representative of the general population may be correct, but it could also be way off. A suggestion that this may be the case is that in places with high infection rates where randomised antibody tests were done such as Stockholm and New York City, the highest positivity rates were around 20%
Secondly, there is no scientific evidence yet that a significant proportion of people testing positive for antibodies, have even short-term, let along long-term immunity against SARS-CoV-2. While there are very strong indications that while re-infection of people who have tested positive for active virus does happen, but is rare, the same has not been shown to be the case for people who have tested positive for the presence of antibodies.
What is happening in Lombardy, Italy, right now, should be warning against writing articles expounding herd immunity related hypotheses without very prominent “NOT PROVEN SCIENTIFICALLY yet” warnings: In June there were reports of 57% of people having antibodies in the Bergamo province in Lombardy, Italy. This is very close to the 70% number to achieve herd immunity often mentioned. It should have been impossible to have the rampant outbreak happening right now, if the hypothesis was correct that presence of antibodies in a large % of the population will result in a low infection rate in a new outbreak. Yet the infection rate in Lombardy is growing exponentially again, doubling in a single day last week, and temporary hospitals in Bergamo and Milan are opening again.
My family and I wear masks. If we eventually learn that it was unnecessary or ineffective, so what? I’m willing to endure a slight inconvenience and discomfort because what if masks are proven to be an effective prophylaxis after all. A slight discomfort compared to what… an at risk person’s death? It is unconscionable.
Can we expect an apology and retraction for an article claiming and telling the public there can be no second wave in South Africa?