SPOTLIGHT
Broken babies, dying patients as North West hospital crisis deepens

Doctors at Mahikeng Provincial Hospital are seeing a rise in the number of infants presenting with brain damage. They correlate the spike with the months-long steady decline and eventual shut-down of the operating theatres in August and September… And this is just one of the problems at the beleaguered hospital.
Dr Zee* unzips her handbag. There’s hand cream and house keys, there’s also nebulising solution, a urine sample bottle half-filled with hospital hand sanitiser, gelcos for administering drips, and other supplies. This is what she calls her crisis management bag.
“All the doctors have this because there are no regular supplies in the hospital. If you see that another department has stock of something you take a few because you can’t be sure your department will have it the next day. We even call this ‘bag stock’,” says Dr Zee, who is based at the troubled Mahikeng Provincial Hospital in the North West province.
Dr Zee is conducting this interview in her car. The car doors are open in hope of a breeze on a baking hot day in the North West. There isn’t a tearoom or rest station for doctors at the hospital. A tearoom is the least of her concerns though, because her and other doctors’ everyday reality now is at best, trying not to be swallowed in the abyss of deepening crisis. At worst, it’s the days she goes home and just bursts into tears.
“It breaks your spirit because you know that day you couldn’t help the patient in the way that they needed to be helped,” she says.
North West state doctors who spoke to Spotlight said their reality has become finding coping mechanisms to process the noticeable spike in brain damaged babies who are arriving in the paediatric wards. Doctors trace it back to when the Mahikeng Hospital theatre services were interrupted last year and limped along to a complete halt for two months in August and September this year.
“Many pregnant women who needed Caesarean sections couldn’t get them in time and were stuck in prolonged labour,” says *Dr Kay, another Mahikeng Provincial Hospital doctor. He confirms that on any given day there are at least three babies here with some kind of brain damage at the hospital.
Physical trauma from prolonged labour (more than 20 hours), including excessive pulling, abnormal use of birth-assisting tools and extended periods of pushing and contractions can cause the baby’s head to be constantly knocked against the mother’s pelvis or be compressed unnecessarily. This has the potential to cause brain damage. When labour does not progress the baby can also become starved of oxygen and suffer perinatal asphyxia, which can also lead to brain damage.
Doctors highlighted a recent case of a baby delivered weighing 5.2kg – he was too big and his mother should have had a C-section. The baby was born with a broken arm which occurred during the very difficult natural birth.
Mahikeng Hospital’s operating theatres have only just started to run again. There’s only a temporary air-conditioning unit in place instead of a specialised chiller unit. It’s a stop-gap measure after services here came to a complete halt for two months.
At the time all four Mahikeng hospital theatres were shut down because the chillers and autoclaves were broken. Chillers are the specialised cooling systems that control temperature and humidity. Autoclaves are sterilising units that keep medical instruments free of bacteria to help control infection. Both are essential in any operating theatre.
“When patients were being transferred to other hospitals (because Mahikeng theatres were shut down) it wasn’t always a good thing because it overburdens other hospitals. We also know that sometimes our patients are victimised when they get to another district. We have already lost track of some patients – we don’t know if they had their operations, if they’re doing well or if they had complications,” says Dr Kay.
The theatre crisis put the Mahikeng crisis on the radar, but Dr Kay says it’s just one of many failings. As Dr Kay talks, his phone bleeps with a message from a colleague. It’s a photograph of a list of supplies in shortage. It includes linen savers to gloves, antibiotics, anaesthetic drugs, antiseptics to sutures and dial-a-flows, the crucial device that regulates the drip rate of a medicine, which is being administered intravenously.
“We haven’t seen a dial-a-flow here for ages. Nurses administer drips and leave it for half an hour in the hope that the patient gets the right dosage. If she forgets about it the patient could overdose, or not get enough of the drugs – it can cause death,” says Dr Zee.
Mahikeng hospital has 392 beds and was built in 1966. Just under 500 patients go through its doors on an average day. In total there are 1 200 employees. A few decades ago its arcaded waiting area at the entrance of the hospital may have been welcoming, pretty even. Now it’s weary and sad. People sit on the floors propped up against the walls. Peeling paint, ageing posters and faded murals tell a story of neglect.

Repairmen work on one of the boilers at the Mahikeng Hospital. Staff say the boilers keep breaking and servicing never sorts out the problems permanently.
In another part of the hospital workmen are repairing a boiler. It looks like maintenance, but nurses laugh, saying it’s another patch-up job. The boilers will be fine for a few weeks maybe, then they’ll break again and the same repairers will be called out again, they say. It means there is often no hot water in the hospital. Some days there’s no water at all, staff say.
There are also no blood culture collection bottles so infections can’t be tracked. The adult wards are next door to one for babies – it’s a breach of infection control. Bio-waste medical boxes are stacked up in the passage and oxygen tanks are dumped near outdoor walkways.
Hospital insiders speak of irregular spending; continued bad management decisions; and administrative hiccups. They include overtime pay not being sorted out to stalled promotions that keep pay grades down, cronyism and bullying from the district and provincial structures. The allegations range from ambulances being misused to transport stable patients or a casualty department upgrade that cost millions, amounting to little more than a fresh coat of paint. All the while there are not enough oxygen points in casualty and patients are still seen in corridors with no triage procedure to prioritise care.
Staff speak under anonymity – there’s a culture of victimisation and intimidation. They are terrified and resentful.
“The MEC addressed doctors here a few weeks ago and he didn’t care about what some people were saying about the mental health and morale of the staff. People even walked out as he was speaking. He essentially said “we know there’s a problem, we can’t fix it, deal with it”. He also blamed us for scaring the public by going to the media.
“But the North West Department of Health can’t hide behind doctors’ and nurses’ silence any more,” says Dr Zee.
By the end of April this year the North West Department of Health was placed under national administration. This came after weeks of violent service delivery protests, labour action led by Nehawu (National Health Education and Allied Workers Union) that started with pharmacy depot workers but spread to include other general health workers. At the same time there were parallel protests across the province calling for then premier Supra Mahumaphelo, to step down. Hospitals and clinics were barricaded, looted and vandalised. The South African National Defence Force health services had to step in to run hospitals, including Mahikeng. They also had to use their medical supplies to supplement the shortages caused by the strikes.
A bed and the basics stand in for a specialist consulting room at Mahikeng Hospital – there’s not even a curtain for privacy.
Jeanette Hunter, the Administrator seconded by the National Department of Health, says it will be 18 months before there’s any noticeable change at Mahikeng.
“There’s been years of decay and Mahikeng is just one of 23 hospitals in the province in need,” she says.
She admits there are “a million things going wrong” but she believes they are on track. She lists infrastructure and addressing staff shortages as priorities, along with reforming the tendering process.
“We know the chillers at Mahikeng have not been properly maintained for years. I had hoped they would limp along till we had a proper tender in place. We can’t carry on with a situation where work is not done to specifications, but we still owe suppliers money,” says Hunter.
Her catch-22, she says, is that she has to continue with irregular spending to keep things just-about running. Irregular can be defined as for example spending on a temporary fix of a split-unit air-conditioning system for Mahikeng’s operating theatres. It does not meet the specifications of a theatre chiller unit and will have to be replaced, but in the short-term it means the surgery schedule can be restarted.
According to the manager of a private air-conditioning company in the province that has experience providing services for hospitals, theatre-grade systems are fitted with specials screens and filters to limit infection risks.
“We’ve heard stories of hospitals hosing down old filters instead of replacing them. The problem is that tenders are given to people who have connections, not necessarily expert knowledge or good standing to do the work properly,” the man says.
“Hospitals don’t pay suppliers for years and they don’t stick to mandatory servicing, which is what keeps systems working efficiently over time,” he says.
Hunter says she hopes to weed out misuse of funds and wasteful expenditure. In her cross-hairs already are those who authorised upgrades for the operating theatres at the JST Hospital in Rustenburg.
“It looks amazing, but nothing works properly. We are investigating and hope to criminally charge whoever’s responsible,” she says.
She adds that Mahikeng’s problems are compounded by the fact that there isn’t a permanent CEO and confirms that a sessional doctor acts as clinical manager.
“No one wants the job because they know it’s a poisoned chalice,” she says.
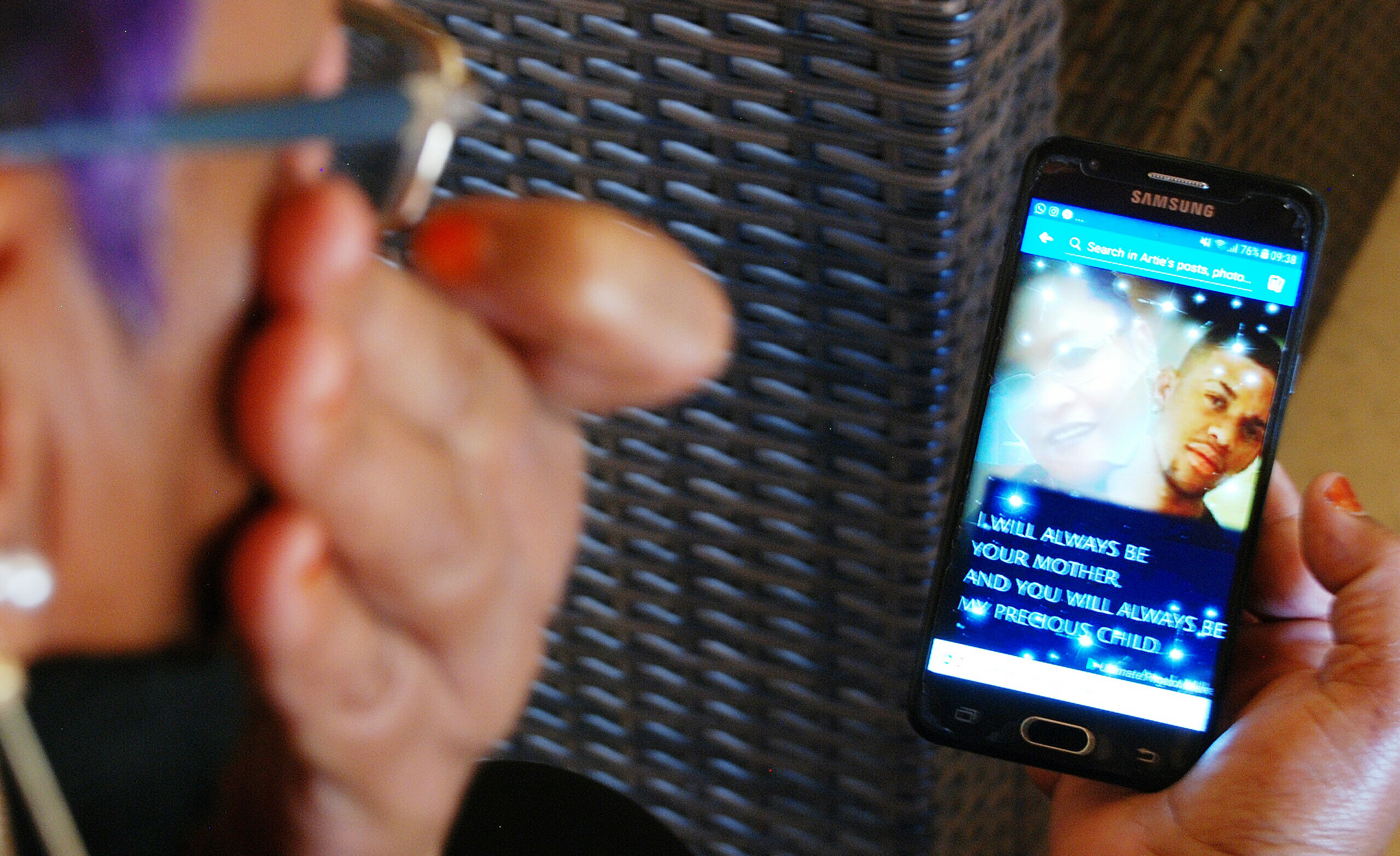
Shaheeda Smith wipes away a tear looking at a photo collage of her and her son Fazeeth. He died in the Mahikeng Hospital.
Hunter calls her job hell, but she’s also not a quitter, she says. Positives, she says, is that she has the backing of both provincial and national treasuries. The budget she has is R11,121-billion this current year. Posts have already been advertised and emergency budgets for purchasing supplies have also been approved.
“It’s not that we don’t have the money. I just need time because we are trying to undo at least a decade of decay while dealing with things like the aftermath of the unrest and protests that affected the province’s hospitals earlier this year,” she says.
When Spotlight visited, the acting CEO at Mahikeng Hospital was Koketso Gopane, the Deputy Director of Corporate Services. Gopane and Matron Lingiwe Dibiga, who at times also occupies the CEO seat, want to believe that Hunter’s turnaround plan will work.
But, even the ad hoc nature of this key leadership position, means there’s no continuity, no oversight and just more complaints and more demands laid at their door.
“Morale is down, down, down, we can’t lie about that,” Gopane says. She tells how in August a security guard go-slow left staff feeling unsafe and intimated at work and meant some staffers ended up volunteering to stand guard.
Dibiga and Gopane say that without a district hospital they are straining under the patient load.
“There are 92 clinics in this district, but people will come here in numbers after 5pm because they want to see a doctor, then they complain when they have to wait a long time,” says Dibiga.
The OPD entrance overfills to the outside walkway. Some people just sit on the floor.
Neither of the acting CEOs have records of the rise in number of brain damaged babies or about the misuse of ambulance services. Dibiga also claims that many complaints about professionalism and unsanitary wards and toilets are exaggerated. She also says patients should take better personal responsibility to keep facilities clean.
Back in the parking lot, Dr Zee is knocking off for the day. Her route home may take her past the sprawling new campus of the Bophelong Psychiatric Hospital. It was supposed to improve access to mental health care and free up the old site for expansion for the Mahikeng Hospital. Six years later, and at a cost of R478-million it’s still not fully functional. Dr Zee may have reasons to cry this day after all. DM
*Identities withheld.
Shaheeda Smith’s story
It’s difficult for Shaheeda Smith to look at photos of her son Fazeeth. He died in December last year. She was at his side, screaming for help as Fazeeth, an asthmatic, died in casualty of the Mahikeng Provincial Hospital.
She scrolls through photos of him on a phone as she recounts events that day. “I ran in screaming for help. Nobody treated it like an emergency,” she remembers.
“The nurses kept asking me ‘where’s his file’ instead of giving him oxygen. They eventually gave me a wheelchair and my husband and I tried to lift him into it,” she says.
Eventually they bought a hospital bed and wheeled the 19-year-old in. A doctor arrived but Shaheeda says she just took her son’s file and disappeared. Later they heard that the doctor had left to make a call to the doctor who had seen Fazeeth when he had an asthma attack earlier in the year.
“How could she go and make a phone call, while my son was dying?”
The minutes wasted away and so did Fazeeth’s last and final breaths. He died suffering and suffocating.
Shaheeda can’t hold back her tears. It was perverse torture that this month (October) she ended up in Mahikeng hospital again, this time as a patient.
“I had a panic attack thinking that I had to go back there. My blood pressure went through the roof,” she says. Five years earlier Shaheeda had an hysterectomy at Mahikeng Hospital. Remembering the after-care she grimaces. She says patients in her ward had to share a single basin of water. Dressings and drips were done incorrectly but “rude, unfriendly” nurses refused to redo them; and wards and toilets were filthy and bloody.
She didn’t realise until she started suffering with abdominal pains earlier this year that she had in fact only had a partial hysterectomy. Her private gynaecologist confirmed that she had two cysts on her ovaries that had to be removed.
“I thought how can I be paining like this but there’s supposed to be nothing inside me? I’m in pain all the time. I stopped walking to work, because half way to work I would feel like my insides are coming out. It’s like labour pains,” she says.
Shaheeda was scheduled for an operation on 8 October at Mahikeng. She arrived before dawn on the day. She shows Spotlight photographs she took of the women sitting on the floor because there were no chairs. At about 9am a doctor came to see them. She and two of the women were told instead they should fill out complaint forms because they would not be operated on that day. The operating theatres had been shut down for two months and they had only that week started working through their backlog.
“We weren’t given a return date or nothing and when we got to the nurses to fill out a complaint, they told us it’s no use, and we should just go home. The girl next to me had a contraceptive loop in her and had been bleeding for three weeks. When you looked at her palms it was like there was no blood in her body. She was just crying and crying,” a horrified Shaheeda recalls.
Shaheeda has not gone back to hospital and survives on painkillers. Her employer is trying to have her admitted to another hospital in the province.
She’s rubs her belly unconsciously every few minutes that she speaks. It hurts, but she’s given up trying to get help and refuses to go back to Mahikeng – it’s tied up in too many painful memories.
“I don’t know if I’m going to make it, but I’m not going back there again. I’ve already written letters to everyone to say goodbye”. DM

















 Become an Insider
Become an Insider